Annual Report 2022-3
Contents:
Welcome to our second Annual Report.
We have made great progress this year building our connections across the kidney community and helping teams put our shared plans into action.
In pursuit of improving quality, outcomes and experience for our patients, our core purpose to show what good looks like, to highlight variation and support teams to improve remains at the centre of our work.
We are grateful to our team of inspirational clinical chairs leading each of our workstreams ranging from prevention in primary care, through to transplantation and dialysis at home.
The quality of our data and reporting has improved significantly this year and we now have really clear evidence of where to focus our attention.
Developing our collaborations
We heard great feedback from people who joined our meetings, groups and online events this year. We know you value the opportunity to meet, talk and share ideas:
-
- Our Transplant team launched our formal collaboration with NHSBT improving access and outcomes
- Over 70 people joined writer and alternative thinker, Matthew Syed, helping challenge our thinking on cognitive diversity and learning from mistakes
- More than 340 colleagues joined our webinars on CKD prevention and early intervention in primary care
- We strengthened our collaboration with ICBs building closer ties with primary care teams and helping create local networks
Discovering new insights
Bringing patients and subject matter experts together we have learned more about our services to inform future priorities:
-
- A virtual Green Nephrology webinar explored options for creating a more sustainable service.
- We brought AKI experts together to understand options for future interventions.
- Our first Young Adults survey highlighted gaps in service and clear inequalities.
- A survey and round table conversation focused on psychosocial wellbeing created a sobering assessment of the shortcomings in currents services and set direction for future work.
Creating guidance
Our focus on collaboration and discovery led to publication of new guidance and advisory reports:
-
- The CKD pathways and coding CKD guidance for primary and secondary care. “3 key actions in 3 months” is a significant step towards delaying progression of kidney disease.
- The LKN Health Equity Audit 2022, created in collaboration with Public Health England (now OHID). This comprehensive assessment of health inequalities through the entire pathway highlights the stark inequalities in access to kidney services and variation in outcomes.
- Integrated pathways for Supportive Care and Advanced Care Planning to guide improvement in symptoms management.
- Guidelines for reimbursing patients for the energy costs of dialysing at home.
Looking ahead
Our work with partners to promote integrated prevention, and seek investment in alternatives to in-centre dialysis resulted in NHSE confirming renal care as a strategic priority for London.
We worked closely with the five ICBs to create proposals to promote predictive, proactive, preventive care and, with NHSE financial support, pilots will start across London during 2023/24 and continue for two years.
Our work to develop demand and capacity planning will continue to create a more resilient dialysis service with improved patient experience.
We will also be strengthening our patient involvement, working more closely with Kidney Patient Associations, and developing peer support in association with Kidney Care UK.
Thank you
The heart of the LKN is our people, our partners, and our patients.
We offer a huge thank you to everyone who has contributed to our work this year as part of our collective endeavour to improve kidney care for our patients.
We look forward to going from strength to strength in the year ahead.
Overview of the LKN
London Kidney Network is improving population health through:
-
- Quality and outcomes
- Health equity and patient experience
- Value and cost effectiveness
The LKN is the largest of 8 formally mandated renal networks in England.
Set up as part of the Renal Services Transformation Programme, supporting the national NHSE Renal “Transform” CRG and implementation of the 100 Renal Medicine GIRFT recommendations at London regional and local ICB level.
The RSTP is a National multi-agency whole-pathway collaboration. It aims to deliver 10 high impact changes to deliver patient-centred care in four domains: Equity of access; Quality of care; Quality improvement; Value in healthcare.
The core purpose of the LKN is to define what good looks like; highlight variation; develop strategy and support delivery of improvement.
There are
people in London living with Chronic Kidney Disease
London has around 15k prevalent renal replacement therapy patients.
- 6.5k people are on haemodialysis
- 15.2k people have end-stage kidney failure
- 8.7k people have had a kidney transplant
Data from the UKKA Patient Reported Experience Measures (PREMs) Survey shows patient experience is poorer in London in key metrics, such as shared decision making.
London and Surrey’s
renal units provide care to
26%
of Englands
in-centre
haemodialysis
patients
The seven adult renal centres deliver dialysis in over 45 units, delivering care to around 5,800 in-centre haemodialysis patients.
At the current rate of dialysis growth, London could have an extra 700 dialysis patients in 10 years’ time.
This would require additional capacity equivalent to Kings to accommodate.
Our system partners
6 Integrated Care Systems
-
- North East London Health and Care Partnership
- North Central London Partners in Health and Care
- North West London Health and Care Partnership
- Our Healthier South East London
- South West London Health and Care Partnership
- Surrey Heartlands Health and Care Partnership
7 Renal Units
-
- Barts Health NHS Trust
- Imperial College Healthcare NHS Trust
- Royal Free London NHS Foundation Trust
- Epsom and St Helier University Hospitals NHS Trust
- St Georges University Hospitals NHS Foundation Trust
- Kings College Hospital NHS Foundation Trust
- Guy’s and St Thomas’ NHS Foundation Trust
How we work
6 agreed Priority Workstreams (3 under development)
4 Expert Advisory Groups
3 Cross-cutting themes
Clinical Workstreams

Preventing Progression

Peritoneal Dialysis

Young Adults

Vascular Access

Transplant

Supportive Care
3 under development: AKI, Psycho-social Support & Well-being, Green Nephrology
Expert Advisory Groups

Clinical Information Group

Health Equity Group

QI Faculty

Patient Partnership and Engagement
Cross-cutting themes

Workforce

Demand & Capacity
LTC network integration
Meet the Team
Clinical Leads

Rob Elias
Clinical Lead

Andrew Frankel
Senior Clinical Advisor

Ravi Rajakariar
Deputy Clinical Lead
Multi-Professional Leads
Workstream Chairs
Expert Advisory Group Chairs
Programme Team
Summary Plans for 2022-23
Transforming Long Term Condition care through an integrated approach to population health improvement across London and Surrey
“Defining what good looks like; highlighting variation; and helping deliver improvement”
Prevention and Early Detection of CKD
- Working across Primary and Secondary care, leading system integration
- Developing Pathways for management and referral
- ICS based CKD /CVD pilots
- Creating consistency in coding and reporting
- Working collaboratively to implement NICE guidance
- Aligning with Diabetes, Cardiac and LTC Networks
Treatment and management of kidney disease
Transplant
- Encouraging a ‘Transplant first’ approach to improve access and outcomes
- Improving equity of access for target populations
- Promoting living donation in high-risk populations
- Promoting a ‘One-London’ approach through unified pathways & mutual aid
- Increasing transplant activity in London
Vascular Access
- Improving timely referral to optimise access
- Introduce principles of 18-week pathway
- Developing a single e-referrals system
- Improve needling access and reduce needle site infections through the MAGIC programme
- Improve day case rates and pathway efficiency
Home Therapies-PD
- Increasing incident PD start rates, reducing reliance on in-centre haemodialysis
- Reducing peritonitis infection rates
- Defining workforce and education needs
- Reviewing patient training models
- Reducing inequity in access to PD
Young Adults
- Agreeing a London pathway and service model
- Supporting Young Adults to live well with renal disease
- Enabling better health, social and educational outcomes
- Proactive management of the consequences of renal disease: e.g. cardiac and psycho-sexual outcomes
- Integrating pathways with Paediatric care providers
End of life & Supportive Care
- Agreeing a London-wide pathway
- Agreeing, collecting and using data to demonstrate need and improvement
- Agreeing workforce model
- Reducing hospital admissions and bed days in last year of life
- Identifying frailty and delivering interventions
- Supporting use case model for the Universal Care Plan
Improving outcomes, experience and value through cross-cutting themes – integrated with LTC networks across London and in ICBs

Patient Partnership and Engagement
- Placing patients and experts by experience at the centre
- Patients in each workstream, with structured development
- Promoting peer support
- Responding to PREMS and PROMS
- Tiered approach to allow optimal input from multiple user groups
- Creating patient resources to empower decision making
- Collaborating with local community groups, faith leaders

Health Equity
- Seeking to improve population health across London
- Evidence based approach through LKN Equity Audit 2022
- Using data to highlight equity gaps and improvement opportunity
- Creating a tool-kit to support improved equity day-to-day
- Development of patient-held equity passport
- Encouraging Equity Pledges

Creating an empowered workforce
- Mapping workforce needs across end-to-end kidney pathways (with HEE and NHSE)
- Supporting development of renal clinicians as system leaders
- Creating a QI Faculty and coaching
- Renal medical trainees & GP Fellows in each workstream
- Developing education modules to address confidence & competence
- Supporting GP training to better manage renal disease

Kidney Data Strategy
- Agreeing minimum standards for data capture and reporting
- Working with LHDS to Integrate primary and secondary care data
- Sharing data across ICSs to identify QI potential issues
- Demand/capacity analysis to inform resilience and future commissioning risk strategy
- Align with UKKA and Renal Registry developments

Governance
- LKN Board oversight
- Accountability to National CRG, London NHSE and ICBs
- Support 6 ICS localised renal/LTC networks with shared priorities & workplan
- LKN workplan to assure delivery of national CRG/RSTP and GIRFT plans
- Supporting specialised commissioning delegation
Resourcing Budget
| N | FTE | 2022/23 | ||
| Pay | Clinical Leadership | |||
| Clinical Leads | 4.00 | 0.40 | 48,860 | |
| Primary Care Leads | 6.00 | 0.60 | 110,400 | |
| Workstream/EAG Chairs | 17.00 | 1.70 | 210,611 | |
| Multi-Professional Clinical Leads | 7.00 | 1.60 | 116,413 | |
| Total Clinical Leadership | 34.00 | 4.30 | 486,283 | |
| Total Patient Partnership | 1.00 | 0.80 | 59,337 | |
| Total Clinical and Patient Leadership | 35.00 | 5.10 | 545,620 | |
| LKN Team | ||||
| Directly employed | 6.00 | 4.80 | 402,353 | |
| Seconded/Recharged | 2.00 | 1.40 | 99,648 | |
| Total LKN Team | 8.00 | 6.20 | 502,001 | |
| Total Pay Budget | 43.00 | 11.30 | 1,047,621 | |
| Non-Pay Budget | 75,500 | |||
| Total LKN Budget | 1,123,121 |
Resourcing priorities
The LKN is targeting resourcing to assure delivery of aims and objectives, focusing on:
- Multi-professional, multi-disciplinary leadership
- Building capacity and capability covering
- Distributed system leadership including renal consultants, Primary Care GPs, nursing, AHPs and Health Scientists
- Effective collaboration behaviours
- Quality improvement delivery
- Explicitly resourcing dedicated time to lead Patient Partnership bringing the patient voice into the heart of LKN decision making and activities
- Core LKN team providing leadership, project management, QI and business intelligence support for workstreams and expert advisory groups
- Developing tools to deliver workstream interventions including communications, prevention search tools, health equity audit evaluation and a number of educational resourcing and tools eg supportive care and health equity
Key deliverables and achievements in 2022-23
Transforming Long Term Condition care through an integrated approach to population health improvement across London and Surrey
Prevention and Early Detection of CKD
Prevention
- CKD Pathways & Coding Guidelines integrated into ICS guidelines
- Collaborated with NWL, ICHP AHSN and Discover-NOW team to transform CKD care.
- Secured 7 funded places on the SEL Scale & Spread Academy
- Awarded £250k funding to optimise CKD coding, early detection and management in South London
- 3 presentations at UKKW 2022/23
Treatment and management of kidney disease
Transplant
- 18-week pathway agreed
- Variation in practice between units identified
- Cardiac, vascular and APKD assessment pathways being localised and implemented
- Mutual aid meant 15+ transplants proceeded that otherwise wouldn’t have
- GOLD pilot across three sites to improve pre-emptive transplant rates in Black patients underway
Vascular Access
- Implemented e-referral at one site, with plans to spread in 2023-24
- Agreed urgent and routine pathways
- Identified unwarranted variation in VA access
- Agreed pathway level metrics to demonstrate impact of QI locally
- MAGIC showing improved patient outcomes and experience
Dialysis – Home Therapies
- Workforce report highlighted variation in nursing workforce and practice across London
- Training report showed gaps in how people are taught to use PD
- Home Therapies reimbursement guidelines enabling personalised care at home
- Transport reimbursement for ICHD work started
Young Adults
- LKN pathway agreed
- Service gaps and unwarranted variation identified
- Renal trainee audit identified areas for improvement; education module in development
- Service Specification being developed
- Business case for Young Adult services being developed
- Pathway metrics agreed
End of life & Supportive Care
Supportive Care
- Supportive Care pathway published
- Supportive care data definition and metrics agreed
- Advanced Care Plan tool published
- Successfully bid to integrate renal information into Universal Care Plan
Improving outcomes, experience and value through cross-cutting themes – integrated with LTC networks across London and in ICBs

Patient Partnership and Engagement
- Toolkit developed to enable more meaningful PPIE
- Patient forum to increased numbers working with LKN attended by over 100 people
- Over 200 patients signed up to stay in touch with LKN work
- Developing Peer Support work in co

Health Equity
- LKN Health Equity Audit 2022 published
- Clear examples of unwarranted variation shown
- Multi-professional workshop, including patients, prioritised issues and agreed solutions
- Identified improvement priorities embedded within each Workstream
- Health Care Professional training module development on target

Creating an empowered workforce
- Over 300 sign-ups to CKD webinar for GPs; feedback that it immediately changed practice
- Young Adult training for renal trainees being developed
- Health Care Professional training module on supportive care and advanced care planning on target

Kidney Data Strategy
- LKN Data pack including ICS dashboard published quarterly
- LKN Demand and Capacity model in use – financial savings – supporting delegation
- Collaborated with clinical experts to agree pathway metrics to show impact of QI in 2023-24

Governance
- Workplans mapped against RSTP and GIRFT
- Local renal networks developing in each ICS
- Links established with ICS LTC teams
- Workplans link national, regional and local priorities for delivery
- Engaged with Population Health Improvement Collaboration
Key milestones
April 2022
PPIE lead started full time, leading to a more patient centred approach to our work
June
Hosted a Green Nephrology Event, promoting greener ways of working and kick-starting work with dialysis technicians to reduce water waste.
July
30 people joined an exploratory event to discuss how LKN could begin to work to address AKI in London
PD Nursing Event gathered expert nursing view on PD workforce, and started work on the PD Nursing Workforce report and recommendation.
September
CKD Early Identification & Optimisation Pathways launched via webinar.
Health Equity Audit published.
October
Home therapies reimbursement guidelines completed and shared for implementation.
November
In-person event for 70 professionals and patients, with keynote speech from Matthew Syed, focused on cognitive diversity and learning from mistakes.
Online questionnaire showed significant gap in trainee renal doctors understanding of young adult care.
December
Vascular Access timed pathways launched.
Supportive Care and Advanced Care Planning pathways completed and shared for implementation.
January 2023
First LKN Transplant Collaborative Meeting.
Young adult patient survey highlighted service gaps and best practice.
February
Psychosocial Round Table hosted to agree how to embed psychosocial care into LKN work.
CESEL integrated LKN CKD Pathways into their official CKD Guidelines,
March
Supported ICS bids for Renal 3Ps programme, worth £10m
Coding CKD in Primary Care Guidelines launched across London via a webinar.
Workstream & EAG achievements / challenges 2022-23 & plans for 2023-24
CKD Prevention
Key achievements
Developed and launched ‘LKN CKD Early Identification & Optimisation Pathways,’ and ‘Coding CKD in Primary Care Guidelines.’ Successfully integrated these into official ICS guidelines across London.
Collaborated with NWL ICHP AHSN and Discover-NOW team to transform the CKD care pathway. Currently rolling out tested solutions at scale in NWL.
Secured £250k funding for South London Pilots.
Hosted national CKD webinars and bespoke educational sessions to support implementation of early CKD identification, coding and optimising care.
Secured 7 places at the SEL Scale & Spread Academy to professionally develop the CKD Prevention Team and facilitate implementation of the LKN Clinical Pathways.
Supported ICSs to achieve a confirmed formulary status for Dapagliflozin for the treatment of CKD.
3 oral presentations at UK Kidney Week by the CKD Prevention Team.
Key challenges
Developing engagement and communications strategy.
Slow progress with establishing patient involvement.
Workstream members and primary care had reduced capacity to engage due to competing demands/priorities.
Plans for 2023-24
Continuing working with ICS teams to develop and deliver their CKD plans as part of the Renal 3Ps Projects.
Finalise the ‘CKD Prevention Resources Package’ for primary care clinicians and patients. Share on LKN website. Link with national RSTP integrated CKD toolkit.
Revise proposal for Data at Scale Improvement Project under London Health Data Strategy Programme. Aim is to secure funding of up to £250K.
Work with relevant partners to develop the LKN ICS System Dashboard to include the top four priority CKD indicators.
Transplant
Key achievements
LKN Transplant Collaborative launched in January 2023.
Cardiac assessment, vascular assessment and PKD work-up pathways signed off and being implemented across London.
LKN Team working collaboratively with charity partners GOLD (Gift of Living Donation) to increase living donation transplants in black kidney patients.
London-wide pharmacy guidelines for use of Imlifidase developed and signed off for use across the Capital.
Two patient focus groups held to generate feedback on the Mutual Aid scheme. Agreed actions will be implemented in 2023-24.
Current deceased donor pathway for transplanting and referring centres mapped at in-person events. Full finding will be reported and acted on in early 2023-24
Key challenges
Transition to LKN Transplant Collaborative from NHSBT Pan-Thames Collaborative resulted in short pause in work plan.
Plans for 2023-24
OUG recommendations in ‘Honoring the Gift of Donation’ report included within the 2023-24 workplan.
Identify and utilise opportunities to increase transplantation rates across London to support reduction in ICHD growth.
Support centres and units to develop QI projects to address areas of unwarranted variation identified within the pathway mapping.
Review Health Equity Audit 2022 and prioritise areas of improvement to reduce inequality.
Continue to develop relationships with patient and community groups e.g. GOLD and JHOD to promote and normalise living and deceased kidney donation.
Dialysis at Home/Peritoneal Dialysis*
Key achievements
LKN Guideline for reimbursement of home therapies utility costs completed and implemented in most London renal units.
PD nursing workforce mapped across LKN renal centres and presented to lead nurses and pan-London PD MDT meeting with plans to support gap analysis within each renal centre.
PD training model with key recommendations completed, presented to Unit Clinical Directors and shared with units to promote local QI projects to implement.
PD training model with key recommendations completed, presented to Unit Clinical Directors and shared with units to promote local QI projects to implement.
Key challenges
Renal units unable to meet timescales to deliver solutions to reduce peritonitis rates. Work will continue into 2023-24.
Approach to mitigating against small and transient PD Nursing workforce complicated by competing demands on unit level resources. Will be continued in 2023-24.
Delay in implementation of home therapies reimbursement guidelines in a minority of units.
Difficulties implementing PD workforce (nursing) recommendations to co-create in –house training approach to date. Ongoing with new targets for delivery in 2023-24.
Plans for 2023-24
Evaluate London’s current home haemodialysis service provision and co-create and implement a clear plan to address unwarranted variation.
Create PD percutaneous access training curriculum and pilot in one unit, with an intent to spread and scale if success criteria met.
Ensure Health Inequalities identified in Health Equity Audit 2022 explicitly addressed in all relevant work e.g. PD access.
Create a platform for sharing HHD best practice and promote collaboration and shared learning between LKN renal centres.
Build a home dialysis peer-support group for patients across London.
Vascular Access
Key achievements
Timed pathways for planned and unplanned starts developed and signed off by all London units. Agreed QI priorities at units as a result.
Pathway metrics to show issues and progress with improvements agreed, with plans to start reporting in 2023-24.
MAGIC (Managing Access through Generating Improvements in Cannulation) programme implemented across London, with data showing improved needling technique and patient experience as a result.
Piloted use of Cerner-based system to accurately track patient waiting times across the VA Pathway at Barts. Highlighted improvement opportunities in current pathways and resulted in changes in practice.
Key challenges
Clinician capacity has limited engagement in developing and implementing local QI plans.
Cost to develop Cerner Millennium module for VA for use across London has proven prohibitive to date.
MAGIC programme has now been discontinued by the National Team, leaving a gap in training opportunities, particularly in satellite units.
Plans for 2023-24
VA Nursing Leads will develop a London training and education solution to build on learning from MAGIC.
Development of a toolkit to enable other renal units to integrate the Barts Cerner-based system. This will enable comparative VA data capture across most of London.
Develop and implement a comprehensive and focused set of local QI projects in response to the agreed priorities identified in 2022-23.
Engage with patient representatives to develop co-designed solutions to relevant pathway issues, and to create patient information to support the changes in service provision.
Young Adults
Key achievements
Comprehensive Young Adult pathway completed, including streamlined transition from paediatric to adult services. Provided clarify of required make-up of YA workforce to deliver the pathway.
SpR confidence to meet YA’s needs self-assessed in an online questionnaire. Current and self-identified training needs identified.
User service experience audited in one renal centre. Result mapped to SpR questionnaire results, with clear parallels between the two identified.
Metrics to effectively measure current practice and performance agreed in Steering Group and with Clinical Information Group.
Key challenges
Local financial resources focused on the YA cohort and local business cases to respond to the demands of the YA service.
Long-standing under-resourcing of YA services makes implementation of identified priorities more difficult.
No YA data currently collected or reported, with no national require for such at present.
Plans for 2023-24
Support each unit to improve in line with the NCEPOD Young Adult report. Use a London-wide workshop to share practice and develop joined up plans, with cross-unit support and collaboration at the centre.
Develop outline business case with key requirements to meet NCEPOD and LKN PAthway included. For use as the basis of any local business case development to minimise unwarranted variation.
Map YA psychosocial provision to identify gaps and variation. Seek to create targeted interventions and collaboration between YA specialties i.e. beyond renal within each Trust where possible. Work in close collaboration with LKN Psycho-social Group to avoid duplication.
In partnership with other renal networks, host a YA RSM training day in December Develop bespoke training for YA professionals in collaboration with KCL.
Supportive Care
Key achievements
Developed a Supportive Care Pathway and an Advanced Care Pathway for use across London.
Developed an education module for health care professionals in response to self-identified lack of confidence in discussing Supportive care and Advanced Care Planning.
Began a process of Peer review visits with each unit to support QI priority identification, against Pathway.
Agreed a clear data set, with agreed definitions agreed for the first time.
Develop a set of 4 patient information booklets to support conversation about Supportive Care and End of Life Care, with patient involvement in their development.
Key challenges
Competing priorities delayed speed of delivery of some items.
Plans for 2023-24
Pilot Supportive Care education module in 3 units, and subsequently roll-out across London.
Develop and launch a GP training module on renal supportive care.
Develop and implement use of a set of symptom management guidelines for use in Primary Care, building on work already done at Barts Health.
Continue the peer review process to continue to support local improvements and to chare learning and good practice across London.
Support delivery of the Supportive Care and Frailty aspects of the Renal 3Ps pilots, through the hosting and management of a Community of Practice.
Hold an Audit Day to baseline current practice against agreed data set, and to showcase exemplar work identified in peer review visits.
Patient Partnership Involvement and Engagement
Key achievements
Continuing working with ICS teams to develop aLKN PPIEG developed to support patient partnership within the LKN and its work.
Patient involvement opportunities launch November 2022.
Patient representation in the majority of clinical workstream and one advisory group with a patient representative support group in progress.
Patient focus groups held on various topics including Mutual Aid for transplantation and CKD Prevention pathways.
LKN patient involvement with partner organisations including Discover Now, Prem, NHSe dialysis transport.
LKN patient oral and poster presentations at BTS and UKKW.
Key challenges
Gap in PPI leadership has led to delays in furthering patient engagement and involvement.
Patient representation to be achieved in remaining workstreams.
Wider patient representation remains limited – this needs to be progressed.
Plans for 2023-24
Appoint to patient lead vacancy.
Formalise patient involvement processes including providing role description for the various types of involvement.
Launch a patient focus group membership initiative with the aim of wider London kidney patient representation.
Further develop a LKN – KCUK peer support initiative and collaboration.
Health Equity Group
Key achievements
Health Equity Audit 2022 published. Half-day in-person workshop including patients and health care professionals discussed the findings. They agreed a set of 6 priority areas for improvement as a result.
Health Equity “Improved” qualitative study established and partnerships made with local groups to support the study to be conducted with local communities groups.
Renal health inequalities knowledge audited amongst NHS staff leading the LKN HEG to create an HE e-module to support learning and understanding across all staff groups.
Health Equity Ambassador role created. These voluntary role can be at taken up by anyone with an interested in health Equity, and aims to promote a culture of equity across services and more broadly across London.
Key challenges
Inconsistent engagement and participation with identified priorities to the current challenging healthcare situation.
Difficult identifying appropriate measurement tool to demonstrate impact of HEG across renal units.
Complexities in building relationships with ICB Population Health and Health Inequality leads due to the emerging nature of ICB posts.
Plans for 2023-24
Launch the Heath and Equity e-module for NHS staff in September and begin monitoring pre/post scores to demonstrate impact.
Develop HE Toolkit to support inclusion of HE across all improvement plans.
Investigate the equity usability of the RSTP dashboard to inform development of the next LKN Health Equity Audit.
Promote HE ambassadors within each LKN renal unit to support and promote HE education, including signposting to the e-module.
Measuring Progress: Data and metrics
During 2022-2023 we honed our data reporting to produce a quarterly system dashboard and LKN data pack. This data is being used to help units and ICSs to identify their local priorities and to benchmark between systems.
The London position on 01 April 2023 (or latest nationally available data) against national targets for transplant, vascular access, home therapies and supportive care are shown here and provide the rationale for work into 2023-24.
System Performance Dashboard
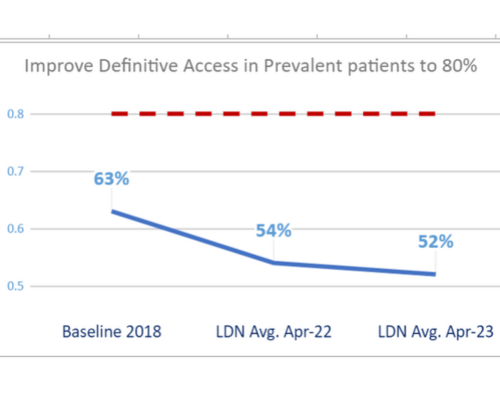
Vascular Access
Definitive vascular access is a well-established quality target in haemodialysis (HD) care and has been strongly incentivised by NHS England by means of a best practice tariff (BPT). Patients without definitive vascular access have higher rates of infection, hospital admission and mortality.
Vascular access surgery and IR intervention can be delivered safely and effectively in the majority of cases as a day case. This facilitates shorter waiting times, improves access to theatre and reduces the likelihood of late cancellation.
Metric 1 – Improve Definitive Access in PREVALENT patients to 80% in each centre
| Target: | Baseline 2018 |
LDN Avg. Apr – 22 |
LDN Avg. Apr-23 |
| 80% | 63% | 54% | 52% |
SOURCE: LKN Quarterly Dashboard
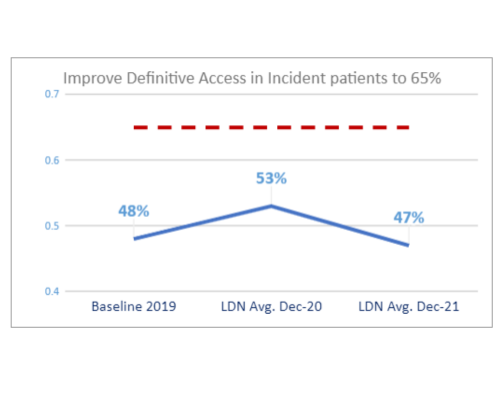
Metric 2 – Improve Definitive Access in INCIDENT patients to 65% in each centre
| Target: | Baseline 2019 | LDN Avg. Dec-20 | LDN Avg. Dec-21 |
| 65% | 48% | 53% | 47% |
There has been a decline in Definitive Access rates since 2018 (see previous slide). This is partly due to the difficulty in improving the Incident Definitive Access rate.
SOURCE: UKKA Annual Report
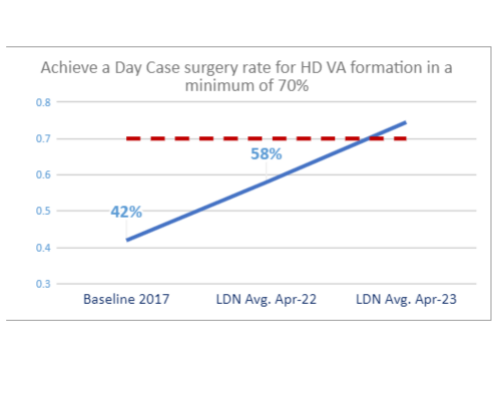
Metric 3 – Achieve a Day Case surgery rate for HD VA formation in a minimum of 70% of all cases in each centre
| Target: | Baseline 2017* | LDN Avg. Apr-22 | LDN Avg. Apr – 23 |
| 70% | 42% | 58% | 75% |
There has been a decline in Definitive Access rates since 2018 but this does not appear to be directly linked to DC surgery provision as this has improved since 2017.
SOURCE: LKN Quarterly Dashboard (*& GIRFT report)
Home Therapies
Home dialysis therapy offers clear benefits in terms of patient experience and quality of life, eliminating the need for patients to travel to hospital several times a week. Given the choice, many would prefer to dialyse at home. These factors provide a strong rationale for improving access to home therapy.
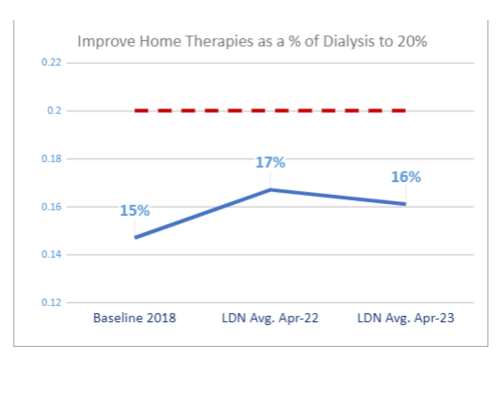
Metric 1 – Improve Home Therapies as a % of Dialysis to 20% in each centre
| Target: | Baseline 2018 | LDN Avg. Apr-22 | LDN Avg. Apr -23 |
| 20% | 15% | 17% | 16% |
Most Trusts saw an uptake in Home Therapies during the Covid period but we are seeing a slight decline again in recent data.
SOURCE: LKN Quarterly Dashboard
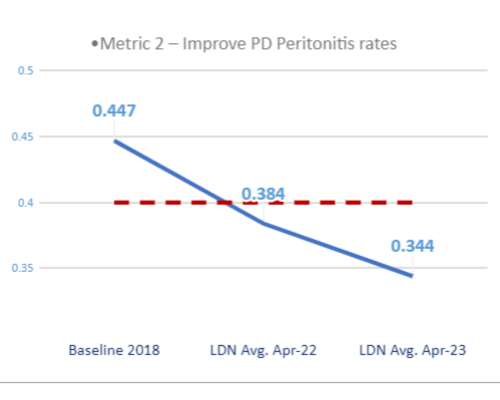
Metric 2 – Improve PD Peritonitis rates
| Target: | Baseline 2018 | LDN Avg. Apr-22 | LDN Avg. Apr-23 |
| 0.400 | 0.447 | 0.384 | 0.344 |
There has been an improvement in the Peritonitis rates since 2018. But it should be noted that this is a lagging indicator (rolling annual average) so any potential impact of the recent PD population growth on Peritonitis rates may not yet be visible.
SOURCE: QSIS Dashboard
Transplantation
Kidney transplantation improves patient outcomes and quality of life, and has significant economic benefits compared with dialysis. Not all patients are suitable for transplantation but there are more prevalent RRT patients with a transplant than on dialysis. A successful transplant means a return to better health and avoids the need for dialysis treatment.
This delivers benefits in terms of better outcomes and cost savings; pre-emptive transplantation avoids both the preparation associated with dialysis (e.g. vascular access surgery) as well as dialysis.
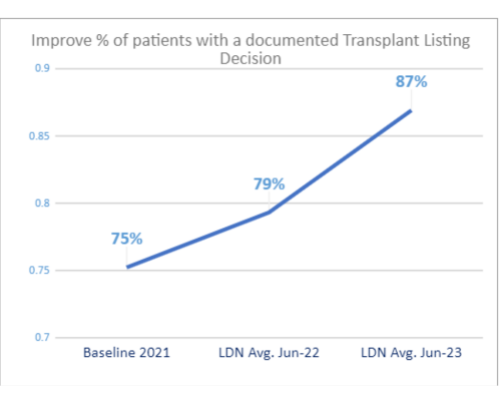
Metric 1 – Improve % of patients with a documented Transplant Listing Decision
| Target: | Baseline 2018 | LDN Avg. Apr-22 | LDN Avg. Apr-23 |
| None | 75% | 79% | 87% |
There has been an improvement in ensuring patients have a documented Transplant Listing Decision. This is an important step in having patients activated on the Kidney Waiting List.
SOURCE: LKN Quarterly Dashboard
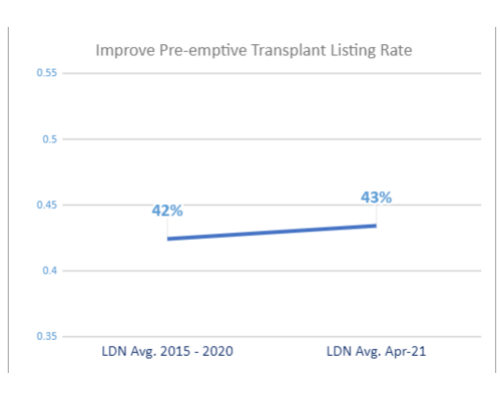
Metric 2 – Improve Pre-emptive Transplant Listing Rate
| Target: | LDN Avg. 2015 | LDN Avg. Apr-21 |
| None | 42% | 43% |
A small improvement on the Pre-emptive Transplant Listing rate. This is an important step in improving the Pre-emptive Transplant procedure rate.
SOURCE: NHSBT Annual Report
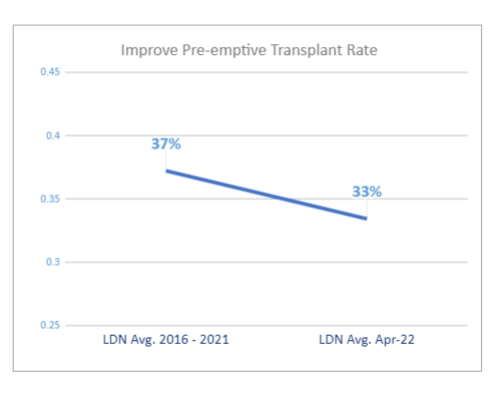
Metric 3 – Improve Pre-emptive Transplant Rate
| Target: | Baseline 2018 | LDN Avg. Apr-22 |
| None | 37% | 33% |
There has been a slight decline in the Pre-emptive Transplant rate as the program works to return to pre-Covid levels.
SOURCE: NHSBT Annual Report
Supportive Care
There are increasing numbers of older, more co-morbid patients with advancing CKD in renal clinics or on renal replacement treatment. Some patients may not benefit from dialysis at all and may have a significantly better QoL on a medical pathway. A supportive care pathway can address the needs of those who will never wish to start RRT, frailer patients in kidney clinics who do plan to have RRT if their kidneys deteriorate, and frailer patients already on RRT.
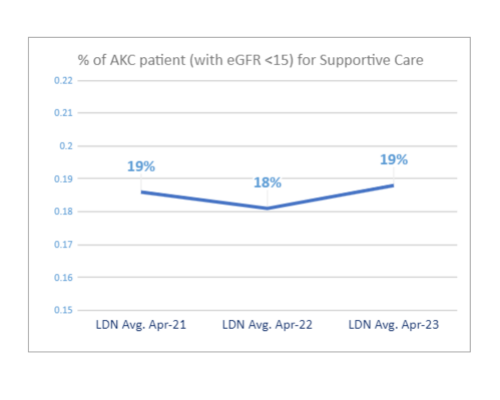
Metric 1 – % of AKC patient (with eGFR <15) for Supportive Care
| Target: | Baseline 2018 | LDN Avg. Apr-22 | LDN Avg. Apr-23 |
| None | 19% | 18% | 19% |
We continue to monitor the Supportive Care population within the AKC cohort. Ensuring that this option is accessible for those who would benefit from this pathway.
SOURCE: LKN Quarterly Dashboard.
Education and Planning events
Identifying, Coding and Managing CKD
9 March 2023
This webinar provided an opportunity to:
✔️ Understand the importance of identifying CKD early
✔️ Learn how to identify and screen those at risk of CKD
✔️ Identify key ways to manage CKD, including medications that protect the kidneys
✔️ Understand the importance of coding CKD and how best to code CKD
✔️ Hear practical experiences and insights from primary and secondary care
It covered
- The Kidney Health Check in adults living with diabetes or hypertension: how to identify CKD early
- ‘3 key interventions within 3 months to save lives’ for adults living with diabetes and kidney disease, or with proteinuric kidney disease
- The new ‘CKD Coding in Primary Care Guidelines – LKN Expert Consensus’
- The role of the nurse/pharmacist
Feedback from GPs who attended
343 people attended and 85 people viewed on YouTube.
CKD Webinar for GPs and Primary Care
7 September 2022
This webinar provided an opportunity to:
✔️ Hear an update on identification and management of chronic kidney disease with the advent of SGLT-2 inhibitors.
✔️ Understand how to implement 3 key interventions in people with diabetic or proteinuric CKD to save lives.
✔️ Explore the critical health inequalities context for chronic kidney disease risk and outcomes in London and Surrey Heartlands.
✔️ Take part in an interactive session where experts from primary and secondary care will be available.
It covered
- Identifying and optimising CKD management early in primary care through the launch of the LKN CKD Early Identification & Optimisation Pathways.
- New approaches to reduce inequalities and save lives.
Attendance
Over 150 people attended and it has been viewed 400 times on YouTube.
“This is easily 1 of the most important educational hours that I have spent this side of the pandemic … I am very keen on the renal pathway and will probably, implement this as a quality improvement program in the practice as soon as I can.”
“This is an epic piece of work … it is well worth the effort.”
“Given all of the other rancour floating around our world, I think you have, in the space of a precious hour within the NHS, enthused me with the thought that I might be able to do some good. Thank you for today.”
Health Equity Audit
11 November 2022
This webinar provided an opportunity to:
✔️ Review findings of the LKN Health Equity Audit 2022.
✔️ Critically appraise findings in groups of experts, including patients, to agree the top 3 priority areas for each part of the patient pathway.
✔️ Agree the key themes and ways to address cross-cutting themes.
✔️ Agree the top 3 priorities to be led by the Health Equity Group.
✔️ Meet as a group, including acute hospital providers, GPs, primary care population health experts, and people with lived experience.
It covered
- Sense checked data and assumptions.
- Explored possible underlying causes of unwarranted variation.
- Presented and discussed emerging priorities.
- Agreed top health equity priorities for each LKN Workstream.
- Agreed overarching health equity priorities to be led by the Health Equity Group across London (Prevention and Early Identification, Practicalities for patients, Improving Patient Health Literacy).
Attendance
30 people attended an in-person afternoon
Feedback
“This is great data. Very interesting and very useful indeed for an overview and broad-brush comparisons.”
Green Nephrology
17 June 2023
This webinar provided an opportunity to:
✔️ Explore why Green Nephrology is important and to plan what we can do to improve.
✔️ Hear examples of national and local good practice.
✔️ Begin to shape a plan to support us all to become greener as individuals, as Units, across ICSs and pan-LKN.
It covered
- ‘Kidney Care in an overheating environment’ Environmental impact of treating kidney disease
- ‘A National View of Green Nephrology’
Initiatives to reduce environmental impact - ‘Examples of Green interventions’
Best practice from Pharmacy, Dialysis technicians, Nephrologists - ‘The patient perspective’ Home dialysis with an environmentally friendly lens to improve patient experience
- ‘Local examples of best practice’
Attendance
35 people joined online
There was collective desire to act. We set up small groups of enthusiasts in professional communities for Renal Technicians share good ideas and help local teams put plans into action through peer support.
“Very insightful and thought-provoking talks, thank you”
“Very motivational and informative, thank you”
Acute Kidney Injury
15 July 2022
This webinar provided an opportunity to:
✔️ Update on AKI service provision in London.
✔️ Bring people together to reflect, learn and action plan.
✔️ Scope and share ideas about what’s working well, and where things could be improved.
✔️ Seek agreement on what interventions might be needed and the timescales for doing so.
It covered
- An Introduction to AKI in London
- RSTP priorities and approach
- London AKI Network (LAKIN)- history, achievements and future
- What does the AKI Data tell us?
- Post-ITU perspective
- Renal Unit feedback and priorities
Attendance
22 joined online
Feedback
“Thank you to the brilliant speakers and great content.”
“Really important and actionable points relating to [the shared] experience.”
Values, Behaviours and Principles Workshop
16 November 2022
This webinar provided an opportunity to:
✔️Explore how the LKN creates value through its collaboration, now and in the future
✔️Develop and align around a set of LKN principles to guide LKN decision making and the behaviours of our members and partners
✔️Determine how we use and embed our principles into LKN ways of working
The workshop was held at the Royal College of Nursing and 19 people attended including, Nurse Leads, Operational and Clinical leads, and Primary Care Leads.
It covered
- Effective collaboration: working with others to create value together, in one of four or more ways.
- Shared voice
- Shared delivery
- aligned plans
- shared learning
- Agreeing the priorities for the LKN: aligned plans and shared learning
- The 8 characteristics of collaboration: agreed we should focus on ways to improve and measure, and ways to communicate and convene
- Development of LKN Principles
Agreed Principles
- Improvement in patient outcomes and experience over all
- Relationships and collaboration over silos and isolation
- Purposeful innovation and improvement over status quo
- Diversity, equity and inclusion over ease and familiarity
- Sustainability and resilience over short term wins
- Flexibility and responsiveness over fixed, rigid mindset
- Transparency over comfort
Quality Improvement with Matthew Syed
16 November 2022
This webinar provided an opportunity to:
✔️ Explore how the LKN creates value through its collaboration, now and in the future.
✔️ Develop and align around a set of LKN principles to guide decision making and the behaviours of our members and partners.
✔️ Determine how we will use and embed our principles into LKN ways of working.
It covered
- Network with colleagues, in-person.
- Understand the value of a systematic approach to improving quality, and alignment to the LKN’s objectives.
- Hear Matthew Syed’s interesting and diverse examples on how and why we should embrace the opportunity before us, using a growth mindset.
- Discuss taking themes, challenges and inspirations back to our units to begin to develop plans to deliver improvements.
Attendance
Workshop was attended by 20 participants, and the engagement event 65 attendees: patients, GPs, Consultants, Nurses, AHPs, General Managers, and ICS leads from across London.
Feedback
“It was thought provoking, and great to see everyone in person.”
“a good opportunity to network, clinically and socially”
“There was a palpable positive energy in the room, and great to see the enthusiasm of people meeting each other face to face. I hope that it acted as a catalyst for some positive action”
LKN Leadership Forum
Monthly learning and sharing
The LKN Leadership Forum runs monthly, and intends to provide a space to share practice, learn from each other, and to share examples of how to embed improvements in day-to-day practice.
The LKN forum had remarkable contributions throughout the year from a wide variety of presenters on topics directly related to the LKN’s priority Workstreams. The Leadership Forum Program and structure were reviewed and formalised from January 2023.
attendees
Vascular Access
23 January 2023
-
- LKN VA data pack quarterly collected, Peter Wilson – LKN BIM
- Implementation of VA pathway at Imperial College Healthcare NHS Trust, Natasha Shenton Deputy General Manager Imperial College Healthcare NHS Trust
- Dialysis Access – Barts Pilot EPR based pathway, Ben Lindsey – LKN VA chair
Nurse “from a practical perspective I welcome the idea of the EPR pw, from a referral point making it so much easier and succinct to the end point you can exactly what specific stage is still outstanding, and I truly welcome the day where we can adopt this across all vascular access nursing. It will our life so much easier.”
attendees
Home therapies – Peritoneal Dialysis
27 February 2023
-
- Reimbursement of utility costs for patients dialysing at home, Richard Corbett – LKN D@H chair
- Improving access to Peritoneal Dialysis, Bhrigu Sood – LKN PD
- Multidisciplinary engagement in the home therapies, Katie Durman – LKN MDT Lead and Babakang Shakoane PD Community senior sister KCH
Audience: “Really excellent work going on in this space and great discussion today. Thank you.” “We’ve made fantastic progress with colleagues collaborating across London, and we’ve seen there is much work to do and we’ve probably sufficient content, expertise and knowledge to translate it into our units.”
attendees
Universal Care Plan
27 March 2023
-
- Overview of UCP
- History
- Current Use
- Future Plans
- System Integration , Lucy Coller, Nick Tigere UCP NHS South West London ICB and Katherine Buxton – UCP, Consultant Palliative Care Imperial College Healthcare NHS Trust
- London Kidney Network (LKN) plans for UCP , Heather Brown – LKN SC chair
Audience: “At the RFL we’re using UCP for conservative care patients already – noting the down the decision not to dialyse. CKD2/3 are mostly not managed by specialists but by GPs and end of life care which is specifically renal would be stage 4/5 patients who have opted not to have dialysis.”
“Amazing work! Look forward to hearing more about how we can ensure this is equitably available and used.” “Excellent work and discussion!”
Other Key Activities and Successes
Demand-Capacity Planning
LKN Demand-Capacity Mapping showed that London’s in-centre haemo-dialysis demand would exceed capacity within 10 years with a predicted associated additional annual system cost of £31.5m. Unit-by-unit mapping showed that in some ICS capacity would be reached within the 2023-24 or early into 2024-25.
This work was instrumental in the development of the Renal Transformation Programme, and will continue to support ICSs to respond to meet local demand in 2023-24.
Renal Transformation Programme
The LKN supported the London ICS’ in developing transformation pilots across the kidney pathway, from prevention to end-of-life care.
The pilots aim to supportive improvement through a proactive, integrated model that delivers population-level improvements.
CKD is one of a cluster of long-term conditions with modifiable risks, along-side diabetes and cardio-vascular disease. This progamme provides opportunity to create a series of pilots to improve outcomes and experience for patients while also reducing whole-system burden of care. These could avoid premature morbidity and mortality associated with CKD and other related high-risk long-term condition, as well as limiting the numbers of people progressing to end-stage renal disease requiring ICHD.
The LKN worked with system leaders to create a Transformation Collaborative to facilitate more efficient utilisation of resources and to fast track shared learning, spread best practice, and gain peer review.
The London ICS bids for one year £1m per ICS non-recurrent funding of transformation were submitted in May 2023. They were all successful, and agreed funding was extended to £2m per ICS over two years. The LKN looks forward to ongoing close working through the Transformation Collaboration in 2023-24 to deliver the first year of activity of these transformative projects.
Plans for 2023-24 and beyond
An integrated systems approach
National drivers:
- National 3 year Renal “Transform” CRG Workplan
- Revised National Service and Network Specification
- NHS 2023/24 Planning Guidance
Local drivers:
- London integration of LTC and Clinical Networks
- Local ICB system priorities for Improving Population Health
- Specialised Commissioning Delegation Preparation & Simulation
Strategic priorities to support system wide approach to Population Health Improvement
| 1 | Demand & Capacity | Create Demand and Capacity plans for ESRF/ICHD, and each pathway stage, for each ICB and renal system to inform service planning, commissioning and delivery. Link future capacity scenarios with LKN Clinical Transformation plans. |
| 2 | Health Equity | Deliver practical actions to reduce kidney health inequalities based on the published LKN Health Equity Audit 2022; focus on integrated approach with LTC networks, GLA and OHID to improve access and outcomes for identified groups |
| 3 | CKD/CVD Prevention | Systematic early identification and optimisation of CKD patients in Primary Care; links with LTC network CVD prevention approaches – cardiac, diabetes, hypertension. Target to optimise SGLT2i prescription for all eligible patients |
Cross-cutting enablers to support strategic priorities
| 4 | Workforce | Develop integrated workforce models with cardiometabolic networks. In liaison with NHSE, HEE and UKKA, develop a strategic renal workforce plan for each stage of the kidney care pathway with all London renal systems. |
| 5 | Data | Optimise primary and secondary care renal data integration (LHDS data at Scale bid); and link with London Data Set developments for other LTC networks and integrated Population health data plans; create the Kidney Health Data Strategy including UKRR daily data feeds; support roll-out Demand & Capacity Model to all renal units & ICS systems |
| 6 | Digitisation | Support expansion of virtual/remote clinic provision and integrated working related to CKD to all renal systems |
| Clinical pathway transformation | Continue with LKN 2022/23 Workstreams and Expert Advisory Group Workplans, adapted to reflect ICS priorities; supporting delivery of pathway and QI priorities from LKN Data Pack, ICS System Dashboards, LKN Equity Audit 2022:
CKD/CVD Prevention – Transplantation – Vascular Access – Home Therapies – Young Adults – Supportive Care |