Annual Report 2023-4
Contents:
Executive Summary
A Year in Numbers

Board Meetings

Workstream Meetings

Education Modules

Renal Transformation Funding

Education Events

Patient Information Leaflets

Datapacks and Dashboards Published

New Data Metric and Methodology Developed

Communities of Practice

Workstreams

Expert Advisory Groups

New Website

Newsletters

Revised Pathways

New Clinical Guidelines and Reports
Welcome to our Third Annual Report
Welcome to our 2023-24 Annual Report.
We’ve had a productive year and hope you’ll enjoy reading about our activity and results. Each section includes a summary of activity and either a case study, or link to the finished work. This year’s report is only available through our website.
A word from our Chair

Dr James Marsh
Group Deputy Chief Executive, St George's Epsom and St Helier Hospitals
2023-24 has been another busy year. It is pleasing to see the breadth of projects that the LKN has supported, ranging from supporting demand and capacity planning to health inequalities and the regional focus on chronic kidney disease and cardiovascular prevention. Much of this was recognised through a series of oral and poster presentations at the UK Kidney Week 2024 in June.
Our clinical workstreams have demonstrated the value of collaboration, shared learning and the community of practice developed across London. I would like to extend my thanks to the LKN team, and our colleagues in primary and secondary care who have collaborated to support improvement and transformation to the way that we provide care to people living with kidney disease.
I look forward with anticipation to further developments in 2024-25
The LKN Team
In 2023-24 we said goodbye to several Team Members. We’d like to thank Bhrigu Sood (PD Access lead), Refik Gokmen (Young Adults Chair), Paramit Chowdhury (Clinical Information Group Chair), Sinead Burke (Multi-professional lead), Conor Byrne (QI Lead), and Victoria Odesesan (Project Co-ordinator) for all their work with the LKN team.
We’d also like to say thank you to our five GP leads. Sarah Morgan (NCL), Neville Pursell (NWL), Vasa Gnanapragasam (SWL), Neil Basudev (SEL) and Chris Carvalho (NEL) have helped the LKN improve primary care support for kidney patients in London. They’ve provided coding guidance, project development, and informed our approach to primary care engagement.
We are delighted to extend a warm welcome to Joyce Popoola (interim Young Adult Chair) and Sarah-Louise Harwood (Patient Partnership and Engagement Lead) who joined us during 2023-24.
You can find full details of the LKN Team here: Meet the team

Programme Team Members

Clinical Leads

Clinical Chairs

Multi-Professional Leads

GP Leads
Summary Plans for 2023-24 by Workstream
Transforming Long Term Condition care through an integrated approach to population health improvement across London and Surrey
“Defining what good looks like; highlighting variation; and helping deliver improvement”
CKD Prevention Workplan
-
- Explore and understand variation in CKD coding, detection and recording in primary care
- Quantify prescription rates of SGLT2i in people with proteinuric CKD, with and without type 2 diabetes (T2DM), to establish current use
- Identify and implement ways to optimise CKD coding, CKD detection rates, and reduce unwarranted variation
- Identify and implement ways to increase SGLT2i use in proteinuric CKD patients with and without T2DM in primary care
- Explore opportunities to develop an agreed data strategy for CKD across ICSs
Transplant Workplan
-
- Implement the 18-week pathway for transplantation across the LKN and its referring centres
- Implement associated pathways i.e. cardiac assessment, vascular assessment, PKD assessment across the LKN and its referring centres
- Fully embed Mutual Aid as BAU and extend the criteria for use
- Map the transplantation workforce and create supporting business cases for use across the LKN
- Deliver three-centre pilot of GOLD programme to increase pre-emptive transplantation in black people
Vascular Workplan
-
- Implement previously agreed urgent and planned VA pathways across the LKN
- Deliver local QI projects, targeted at identified ‘pinch points’
- Deliver MAGIC (Managing Access by Generating Improvements in Canulation) across the LKN, and analyse additional patient experience data
- Complete root cause analysis of low day-case rates with each unit, and develop findings into a case for change with associated timed plans for delivery
Home Therapies Workplan
-
- Define an appropriately trained and resourced MDT workforce that delivers high quality care in community and hospital settings
- Achieve a significant and sustained improvement in peritonitis rates and outcomes
- Define, agree and support implementation of timely access to comprehensive, local, person-centred training for all people starting PD, to increase both prevalent and incident numbers of patients on PD
- Improve access to timely PD catheter insertion and re-insertion, to support prevalent and incident population on PD
- Ensure Health inequality is addressed and not widen through the PD improvement plans
Young Adults Workplan
-
- Enable every Young Adult with kidney disease in London to have access to a Young adult clinic
- Establish a system of routine data collection including patient experience in transition care
- Ensure all health care professionals who have contact with Young Adults are appropriately skilled to provide best-practice interventions
- Establish and enable young adult patients to have psychological support at London’s kidney units
- Define best practice to optimise medication adherence for young adult patients
Supportive Care Workplan
-
- Agree supportive care definition across London
- Routinely screen patients with CFS (Clinical Frailty Score) and SQ (Surprise Question) to identify those appropriate for supportive care
- Routinely collect and report supportive care data
- Train renal workforce to confidently discuss supportive care with patients
- Ensure Supportive Care training and education module is used by staff in all London renal units
- Deliver GP Training package on renal supportive care across all ICSs
- Support use of LKN Supportive Care Patient information leaflets
- Develop business cases for additional Supportive Care staff resource
- Deliver project with UCP (Universal Care Planning team)
Patient Partnership Involvement Engagement (PPIE) Group Workplan
- Provide guidance and support materials to enable those within workstreams to conduct PPIE activities
- Provide regular ongoing support to workstreams
- Develop a review process for each workstream to share learning, successes and challenges of PPIE activity
- Assess utility of support materials developed
- Develop communications plan for patients
Clinical Information Group Workplan
-
- Continue to develop the quarterly Data Pack and Summary Dashboard that will act as the KPIs for the network and reflecting the individual Trusts service delivery and stated aims of equity of service
- Continue development of an LKN Demand & Capacity Model allowing for 5 & 10 year+ forecasting of dialysis & ICHD demand linking this with resource (workforce, estate, capital) need
- Develop a London Kidney Health Data Strategy
Health Equity Expert Advisory Group
-
- Deliver targeted health equity improvement across the LKN to assure inclusive and equitable access for all kidney patients
- Highlight existing inequalities for people with kidney disease and support the kidney workforce to address and reduce the impact of these in their daily practice
- Create a live inventory of pilots and best practices to be used as a resource for LKN service groups including patients
- Develop research priorities to improve health equity in renal care within the LKN units based on local data and informed by health equity priorities for patients and health care professionals
Workstream Successes and Achievements
Preventing CKD Progression
The LKN Preventing CKD Progression Workstream completed several key pieces of work during 2023-24
- The CKD early identification and optimisation pathways were updated. You can find them here: Preventing Progression
- The LKN CKD resources packages (co-created with patients, clinicians and Kidney Care UK) provide a single source of trusted information for primary care and for patients, found here:
For primary care clinicians: Resources
For patients: Resources - The LKN worked with the North West London ICS and Imperial College Health Partners on a 2-year project to transform early identification and management of CKD. Solutions were co-designed with clinicians, patients and digital/service design experts. Implemented solutions include searches, guides, dashboards, educational resources, automated coding guidance, diagnosis pathway, alerts and templates. Project details and all these solutions are available here: Learn more
- SGLT-2 inhibitors (SGLT2i) are medications that slow progression of kidney disease and reduce cardiovascular events. The LKN CKD Prevention Workstream worked closely with ICSs (including medicines optimisation committees) to support primary care to initiate SGLT2i for CKD.
Transplant
Following co-Chair recruitment, the Collaborative has worked to develop and embed delivery of key transplant priorities for London.
Referral Pathway Mapping
- The Collaborative mapped the patient pathway from AKCC (Advanced Kidney Care Clinic) to transplant decision in the London transplanting centres and their referring units (including those outside London). The results have helped to direct the Collaborative’s work and helped Units to develop quality improvement initiatives.
Gift Of Living Donation: Phone Peer Buddy Scheme
- The LKN worked with the Gift Of Living Donation charity to deliver a three-site QI project implementing peer buddy telephone support to increase the number of kidney offers from black living donors. You can find the full project report here: Learn more
Mutual Aid
- Mutual aid is a kidney transplant completed at a London transplant centre which isn’t the patient’s usual treating hospital, and was established during the COVID-19 pandemic
- The Transplant Collaborative sought patient feedback on Mutual Aid, holding two virtual patient focus groups in April 2023; one for those who’d received a transplant and one for those who hadn’t
- The focus groups agreed that those who may benefit from Mutual Aid should be given information at three key time points: assessment; before transfer to the new transplant centre; and once at the transplant centre.
- The findings of the focus groups are being used to improve patient engagement with the Collaborative, and to support health care professionals give targeted information about Mutual aid at the right time for patients.
Five-year plan for London
The 5 Year Transplant Plan is being developed in partnership with NHSE London. It intends to increase numbers of available donors, ensure equitable access to transplant services, and improve long-term outcomes for those with kidney transplants. The Collaborative held an in-person workshop, attended by 70 people, in March 2024 to further develop the plan and seek feedback on the priorities and actions. A full report can be found here: Learn more
Vascular Access
The Vascular Access Group have worked to identify barriers and drivers to delivering vascular access across the region, including benchmarking, reaching agreement on vascular access pathway standards, and how these can be digitised.
The following case studies show how two Trusts have implemented changes locally as a result.
Local QI using the LKN Vascular Access Pathway
Barts Health NHS Trust
Ben Lindsey, VA Pathway Chair and Consultant General, Vascular and Renal Transplant Surgeon at Bart’s Health has worked over the last two years to develop and embed an e-referral pathway for vascular access. He says:
-
as a proportion of the overall cost of delivering dialysis for 1500 patients (PD and HD), investment in a WTE band four pathway navigator, to effect safe access, was easily justifiable.
-
operating outside of the main theatre suite (the ward AVF programme) was the only way that capacity to create arteriovenous fistulas could be met, as such sessions, in addition to the existing funded job planned activity, were funded to support additional operating time to create AVFs.
-
additional funding would be made available to pay external experts from other trusts to mentor the surgical and medical teams to implement a ward-based PD catheter insertion programme, which includes a new consultant nephrology appointment job plan specifying an interest in this activity.”
This work is being used to support other units across London to develop their own QI with a view to rolling out the e-referral module with all Trusts using CERNER over the coming year.
Imperial College Healthcare NHS Trust
Using learning from the LKN VA Group, Imperial created a vascular access pathway coordinator role. In his first three months in post, Daniel Magdzinski has dramatically improved patient outcomes and waiting times. In addition, the dialysis access clinic DNA rate has dropped by 12%, from 17% to 5%. He is now training members of the wider renal administrative team across NWL about how to manage dialysis access clinics. This will ensure sustainability of improvements in outcomes, and will upskill and support colleagues across the service. Daniel will then focus on other aspects of the vascular access pathway, such as supporting the Vascular Access MDT.
The collegiate approach Imperial have taken with the London Kidney Network has helped them raise the profile of vascular access internally and facilitated improved collaboration with the clinical team, says Natasha Shenton, Deputy General manager. Nadine MacLean, Kidney and Transplant Business Manager, has been key in service improvement within the ICHT vascular access service. Working closely with the vascular access lead surgeon, Mr Paul Herbert, Head of Specialty for Kidney Surgery, Mr Anand Muthusamy, Vascular Access Clinical Nurse Specialist, Saidat Abbas, and Renal Quality and Information Manager, Darren Duffield, Nadine has made significant improvements with the internal vascular access referral and booking processes. As a direct result, fistula creation waiting time has halved, from 12 to 6 weeks, and there is improved oversight and visibility of vascular access referrals from across NWL.
Paul
Consultant Transplant, General and Vascular Access Surgeon, Imperial College NHS Trust
Says “Imperial College NHS Trust cares for a huge cohort of renal patients and the establishment of Daniel’s role and the support of the management team has allowed us to start to make real progress in this area”

Natasha
Deputy General Manager Renal and Transplant Directorate, Imperial College Healthcare NHS Trust
Reflects “The Imperial College Healthcare NHS Trust (ICHT) renal vascular access service has hugely benefited from the LKN VA group, and the impact on patient outcomes is tangible. For example, as a result of shared learning and benchmarking discussions with colleagues across the region, we were able to establish a dedicated vascular access pathway coordinator to support the service. This absolutely would not have been possible without the support of the London vascular access and kidney network, as the shared learning and outcomes from other providers supported the case for change, and the increase in administrative establishment within our service.”
Vascular Access Nurses Training Day
The closure of the national MAGIC programme meant that there was a lack of training available for Specialist Vascular access nurses, and those working in dialysis units who use vascular access sites on a daily basis. To address this gap, an in-person training day, split into a morning for the expert VA CNSs and an afternoon for dialysis nurses, was held. A summary of which can be found here: Learn more
Peritoneal Dialysis/Dialysis at Home
The PD Workstream expanded its remit to cover all Dialysis at Home in Q3 2023-24.
PD Nursing Workforce mapped
To deliver high quality PD services a sufficient and skilled nursing workforce is needed. The current nursing workforce was mapped, showing variation in numbers, banding, service delivery model, and more. The full report can be found here: Reports
PD (Peritoneal dialysis) Access mapping
An online questionnaire was developed and completed by all London units to establish current service provision and to identify unwarranted variation. The results are being used to help direct improvement work in 2024-25. We thank Dr Bhrigu Sood for his leadership and vision on this piece of work. You can find the full report here: Reports
PD Access training package
To ensure a robust and competent consultant workforce, able to deliver PD access catheter insertion, a package of training was developed. It will be piloted during 2024-25 and can be found here: Guidelines
Utilities reimbursement updated
Utility costs for those receiving dialysis at home should be reimbursed. Pan-London guidance published in 2022-23 was updated this year and can be found here: Guidelines
Working with Industry partners to address operational issues
The LKN acted to support the resolution of supply issues with dialysis consumables to both renal units and people doing haemodialysis at home. During late 2023 and into the New Year 2024, operational supply issues at a home therapy service provider led to significant service disruptions in both in-centre and home haemodialysis. The network worked with the provider and network renal units to improve communication, resolve operational issues in a prompt and equitable manner, as well as ensuring the continuity of care of people dialysing at home.
Home HD services mapped
Home HD services were mapped to highlight variations, share best practice, understand demand and delivery differences across London, aiming to support increased Home HD uptake by eligible patients. The full report will be published in 2024.
Supportive Care
The Supportive Care Workstream completed several important pieces of work during 2023-24.
- To get a better understanding of the successes and areas of concern at each unit, the co-Chairs and project manager visited a majority of units’ supportive care teams early in 2023-24. These were useful for all participants and helped shape activity of the Workstream.
- Discussing supportive care as a treatment option with patients requires both competence and confidence. An audit in South London in 2020, showed that many health care professionals did not feel able to discuss supportive care, or advanced care planning. Creation of an e-module for staff was completed this year and is free to access here: e-module
- Short videos explaining Supportive Care and Advanced Care Planning for Health professionals were developed and can be found here: View
- Provision of written patient information is vital during discussion of treatment options and so two booklets were written and published to fill an identified gap. They can be found here: View PDF and here View PDF
- In order to support GPs to better understand supportive care as a treatment choice, a training package was developed and a webinar delivered. You can find the webinar here: View here
- Supportive Care metrics were agreed and audited (see Data in Action, section 6)
- An in-person Audit and training day were delivered in December 2023. Education
Young Adults
Having developed a clear pathway for services in 2022-23, the Young Adults Workstream has focused on how to address the gaps in service access in 2023-24. This will continue into 2024-25.
- A patient experience survey was piloted in one Trust. The results were mapped against the junior Doctor self-reported training and knowledge questionnaire, and showed the same areas for improvement
- A training event was co-developed with TIER* Network and North West Kidney Network, and held at the Royal College of Medicine.
- Young Adult metrics have been agreed and reported on for the first time. This will be refined in 2024-25
- Work has started on a co-designed, patient held passport. This will enable Young Adults attending hospitals other than their treating centre to share relevant information about their care and medical needs in a clear, concise and useful way.
- Previous service mapping identified significant differences in access to psycho-social services. Work has started to seek to reduce inequality of access, sharing learning from other specialities and from kidney units where access is better. It will reboot in 2024-25
*Transition & Patient Empowerment Innovation, Education and Research Collaboration.
(TIER is an international collaboration of healthcare professionals who are passionate about working together with patients and carers to empower children, young people and adults to help manage their condition, promote best practices and share resources)
Health Equity
The Health Equity group have focused on the delivery of two key projects in 2023-24
- Completion and roll-out of the Health Equity e-module. This was designed to help anyone, who comes into contact with a person with kidney disease, to understand how kidney health inequality might affect them. You can find the free, online training module here: Training
- Completion of a toolkit which supports inclusion of health equity actions in all LKN Workstream workplans. The toolkit, and detail on how and why it’s important, can be found here Toolkit
In addition, local Health Equity focused QI projects have been undertaken in response to inequalities highlighted by the LKN Health Equity Group. For example, Dr Ben Oliveira led the implementation of a Making Every Contact Count (MECC) initiative at Barts Health.
MECC Case Study
“Using the support and expertise of the LKN’s Health Equities Group (HEG), a pilot project launched at Barts Health in 2023. It combined staff training in Making Every Contact Count (MECC) with the introduction of a Healthy Living Advisor (HLA) to both record the extent of inequalities and to help mitigate their impact on patients’ health. Funding was sought by the Barts Health Public Health team to enable three renal staff to attend a MECC Train the Trainer programme. In turn these staff were able to train 12 members of the New Starters Dialysis Team at Bart’s Health. Evaluation showed the training increased staff confidence in making brief interventions to support patients to make positive changes in their lifestyle.”
Alongside this, a HLA was introduced, funded by Barts Charity, to support staff working with patients in the New Starters Unit. Between September and December 2023 the HLA screened all 131 patients starting dialysis in the unit. 75% of patients lived in the first (25%) or second (50%) most deprived quintiles of deprivation. Of the 131 patients, 27% reported financial insecurity, 14% reported food insecurity, and 9% reported housing insecurity in the last 2 months.
%
of patients lived in areas with the highest levels of poverty
%
reported financial insecurity
%
reported food insecurity
%
reported housing insecurity
73% of patients benefited from either simple advice, signposting to relevant services or an onward referral to another service. The most frequently requested area of support related to diet, which was mostly through dietitian referral, but also referrals to food banks (10%). The second most common need was financial. People required help with applying for benefits and signposting to grants for kidney patients.
50 patients have been followed up since their intervention with the HLA, 66% of whom were referred or signposted to more than one additional route of support.
Of those, 76% reported that they were either contacted by the service or had made direct contact with the signposted service. 90% of those patients reported that the referral and signposting were beneficial. There was an improvement in mean EQ-5D (a measure of health) score following the intervention; 1.4 before Vs 1.6 after.
The MECC project highlighted the extent of social deprivation for patients newly starting dialysis at Barts Health, with high levels of food, housing and financial insecurity. Further work is ongoing to collect follow-up data for the remaining patients screened. There is also a plan for staff in the Low Clearance team to receive MECC training so that more patients can benefit from this intervention across the Renal service at Barts Health.
Patient Engagement Group
We welcomed Sarah-Louise Harwood to the Patient Partnership Lead role in February. Patients from all kidney units are involved in LKN PPE work, and patient representatives are members of most LKN workstreams and expert advisory groups.
A new initiative to increase patient involvement in the LKN was co-developed by Andrew McAllister (patient representative) and Wendy Brown (interim PPE Lead). The purpose of the Patient Experience Discussion meetings is to share experience with LKN workstream leads, in order to shape workstream priorities to improve outcomes. Following an online launch event in November, the first three months covered:
- Which areas of kidney care feel unequal to patients in London?
- What are your experiences of choosing dialysis treatment?
- What is the patient experience of the transplant pathway?
Around 15 patients have attended each session, with patients self-selecting topics which they are interested in and which they have useful experience to share.
A joint initiative between the LKN and Kidney Care UK developed and co-funded a Peer Support Coordinator for London. Peer Support has been shown to be an important tool in improving outcomes for patients. Deniz Hasan started her role in March, and coordinates the peer support programme across all London renal units. The Peer Support Programme is an essential part of Patient Partnership and Engagement and is fully integrated into the LKN workplan for 2024-25.
We have been delighted to work closely with charity partners and representatives, including the London KPAs (Kidney Patient Associations) through the National Kidney Foundation, Kidney Research UK, and Kidney Beam.
Measuring Progress: Data and metrics
Data is at the heart of the LKN’s work. During 2023-24 Peter Wilson, LKN Business Intelligence Manager, has worked to refine and develop the quarterly data pack and dashboard. It now shows more detailed and nuanced information, providing a clearer picture within units and across London. You can find our data packs here https://londonkidneynetwork.nhs.uk/data/ and if you’d like to see the dashboard, please email us at lkn.londonkidneynetwork@nhs.net
Each workstream has worked to create a more granular and detailed data set to support the LKN Data Pack and Dashboard. For example, Vascular Access reported their agreed data set for the first time in January 2024. You can see a detailed case study of the Supportive Care Workstream’s audit, below.
Data in action: 2 case studies
Creating a Kidney Dialysis Occupancy Measure (DOM) for London
LKN modelling of demand and capacity of In Centre Haemodialysis (ICH), showed demand growth of around 3% per year, with local variation across the seven renal units in 48 locations in London.
Despite best efforts to mitigate this growth – including early identification and prevention, higher rates of transplantation, and expanding home therapies – demand growth will continue. Working with units, we found that use of ICHD estate capacity was at 88.3% (range 73.5 % – 105.4%) and available staffed capacity at 97.9% (range 88.0 % – 103.9%) across the whole of London by mid 2023-24. A problem statement was agreed with Renal Clinical Directors
“Currently, kidney units, London ICBs and NHSE do not have a systematic and unified way of ensuring clear visibility of the capacity pressure or the risks associated with running ICHD services so close to operational safe capacity.”
With clinical consensus and agreement from the London renal unit Clinical Directors and Clinical Leads, the LKN developed a standard and consistent measure of ICHD capacity – the Kidney DOM. It is intended to be simple to use, easy to measure, and easy to report proxy indicators of clinical safety, patient experience and service resilience.
It was trialled and refined between December and February, and is now being reported on a monthly basis, showing reliable, accurate and up-to-date information about dialysis occupancy. The DOM has been included in the NHS London Specialised Commissioning Integrated Performance Report and Kidney Networks across England are planning to start using it during 2024-25.

Mark Kowalczuk
General Manager for Renal Services, Barts Health NHS Trust
Says: “The Kidney DOM has been essential in standardising the way in which we review and analyse capacity across different sites and networks across the LKN. One of the key challenges within dialysis is the amount of data available and the number of different ways that you can assess demand and capacity. Some services review demand and capacity in terms of number of patients, others look at number of slots, some look at sessions provided others use SLAM/commissioning activity data. You can look at physical capacity and you can look at staffed capacity. There are added complications when patients go on holiday or are admitted into hospital such that they are not using their chronic dialysis slots, equally some patients dialyse twice per week as opposed to three times. These are small nuances but can have significant impact when looking at large patient cohorts which are being measured via different metrics. When lobbying for additional investment in dialysis capacity there is an obvious need to demonstrate that you are effectively and efficiently using your current capacity and the Kidney DOM has provided a standardized and regulated means to demonstrate this and has been a great help in securing additional investment in dialysis across North East London.”
To find out more about the Kidney DOM, please contact us on: lkn.londonkidneynetwork@nhs.net
Supportive Care (SC) Audit
There is no nationally agreed supportive care data set, and the only routinely reported data item is percentage of Advanced Kidney Care Clinic (AKCC) patients on a supportive care pathway. The Supportive Care Workstream developed and agreed a data set, in close partnership with the Clinical Information Group, and completed a supportive care audit in December 2023. Data included service information, clinical frailty scoring (CFS), evidence of advanced care planning and mortality. All units submitted data but there was wide variation in data captured and extractability.
To our knowledge it was the first time a Network has collected extensive supportive care data, other than that issued by the Scottish Renal Registry.
Key Findings:
- Patients within AKCC whose chosen modality was RRT were generally younger than those choosing supportive care. They were living with more frailty than those planned for RRT. This suggests where CFS scores were recorded, they may have contributed to pathway choices within AKCC.
- Not all centres in London were collecting CFS data in AKCC, prior to treatment decision. This suggests a possible missed opportunity to provide the most suitable treatment options.
- This was a challenging audit, with inconsistencies and incomplete information. However, it has led to units focusing on identifying those with frailty.
- Additionally, the data has influenced service prioritisation across London. All units now have additional frailty input within AKCC, with planned presence across all renal care.
Work into 2024-25 will include refining the data items, working with units and ICBs to develop solutions to data capture and extractability, and developing improved access to frailty services. Much of this will be through the Renal 3 Priority Programme.

Dr Heather Brown and Dr Katie Vinen
Co-Chairs of the Supportive Care Workstream
Said: “We recognised that with very limited data in this area it was impossible to understand and prioritise the supportive care service or to measure change as we sought to improve it. Although we are still improving data collection in this area, Trust Data Managers are now seeking to automate supportive care data collection and increased visibility for this part of the service is helping us to understand the scale of need and to support improved care in this area”
Collaboration in the LKN
Renal Transformation Pilots – a suite of inter-related pilot initiatives
In April 2023 an opportunity arose to support the London ICS’ bid for funding from NHS England (London) to support transformation change in the renal pathway, with the dual aim of
- reducing the unmitigated growth in in-centre haemodialysis (ICHD), and
- improving patient experience and outcomes
The LKN has worked collaboratively with ICS leads and project teams to:
- Develop the bids
- Identify commonality in approach and methodology
- Shape plans using agreed LKN workstream guidelines and data
- Develop agreed metrics for pan-London analysis of outcomes
- Provide oversight through the London Kidney Transformation Board
Each ICS was awarded £2m over two years to implement their priority projects (see below)
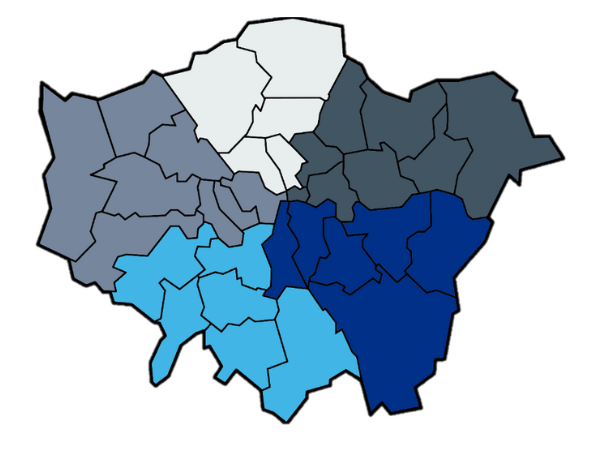
North West (mid grey)
- Primary cardio-metabolic hubs
- Ealing Discover Now
- Patient education and support
- Accelerated pathway for advanced kidney care
- Improving diabetes care in people on dialysis
- Embedding frailty support in AKCC
- Advanced care planning
South West (mid blue)
- Optimising prevention, detection and management of CKD in the community
- Integrated cardio-metabolic MDT approach for multi co-morbid patients (supportive care, complex discharge planning, heart failure management)
- People and community engagement, activation and empowerment
North Central (light grey)
- CKD coding in primary care
- Targeting people at-risk of CKD for eGFR
- Weight loss clinic for transplant eligibility
- MDT approach to increase patient choice and eligibility for alternate therapies to ICHD
North East (dark grey)
- Cardiometabolic approach to early identification and management of risk factors
- Supporting patient-led care (improving experience for late presenters, enhancing a purpose built unit for young adults, embedding frailty input, offering home from home dialysis)
South East (dark blue)
Developing CKD integrated pathways as part of a cardio-metabolic model:
- Prevention and screening
- Community case management and MDT approach
- Secondary care integrated MDT (incl. embedding frailty input in advanced kidney care)
Working with other Long-Term Condition Networks in London
Education and Events

6 in-person events

8 Leadership Fora

1 Webinar

711 participants

60 presenters

33 hours of teaching
Over the last year, we have expanded and developed our leadership fora. In an online survey in November, we asked you what you wanted more of, and what we could improve. We rolled-out the changes in January 2024. You can read the full report in the ‘reports’ section here https://londonkidneynetwork.nhs.uk/our-work/#education
Presenters in 2023-24 have included: Patients, acute care based professionals , GPs, NHS England, ICS leads, and Charitable Sector representatives.
Multiple professions were represented as presenters and participants, including: Doctors, Nurses, Dietitians, Physios, Service Managers, Commissioners, Data Managers, Pharmacists, and Patients.
There was participation and presentations at our fora and education events from across London and Nationally.
Resourcing Budget
Financial position at year end 2023-24
Resourcing priorities for 2023-24
The LKN is targeting resourcing to ensure delivery of aims and objectives, focusing on:
- Multi-professional, multi-disciplinary leadership
- Building capacity and capability covering:
- Distributed system leadership, including Renal Consultants, Primary Care GPs, Nurses, AHPs and Health Scientists
- Effective collaborative behaviours
- Quality improvement delivery
- Explicitly resourcing patient partnership, putting the patient voice at the heart of LKN decision making and activities
- Core LKN team providing leadership, project management, QI and business intelligence support for workstreams and expert advisory groups
- Developing tools to deliver workstream interventions including educational resources e.g. supportive care and health equity e-modules
| Summary | LKN 2023/24 | LKN 2023/24 | LKN 2023/24 | |
| Budget | Q4 | Variance | ||
| Income | (991,108) | (1,014,513) | – | |
| Expenditure | Pay | 986,652 | 858,586 | (128,006) |
| Non-Pay | 46,500 | 64,090 | 17,590 | |
| Total net underspend | 42,004 | (91,837) | (110,476) |
Summary Plan for 2024-25
Transforming Long Term Condition care through an integrated approach to population health improvement across London and Surrey
Connecting | Collaborating | Challenging
Workplan 2024-25
View PDF