London and Surrey kidney facts and figures
London and Surrey kidney facts
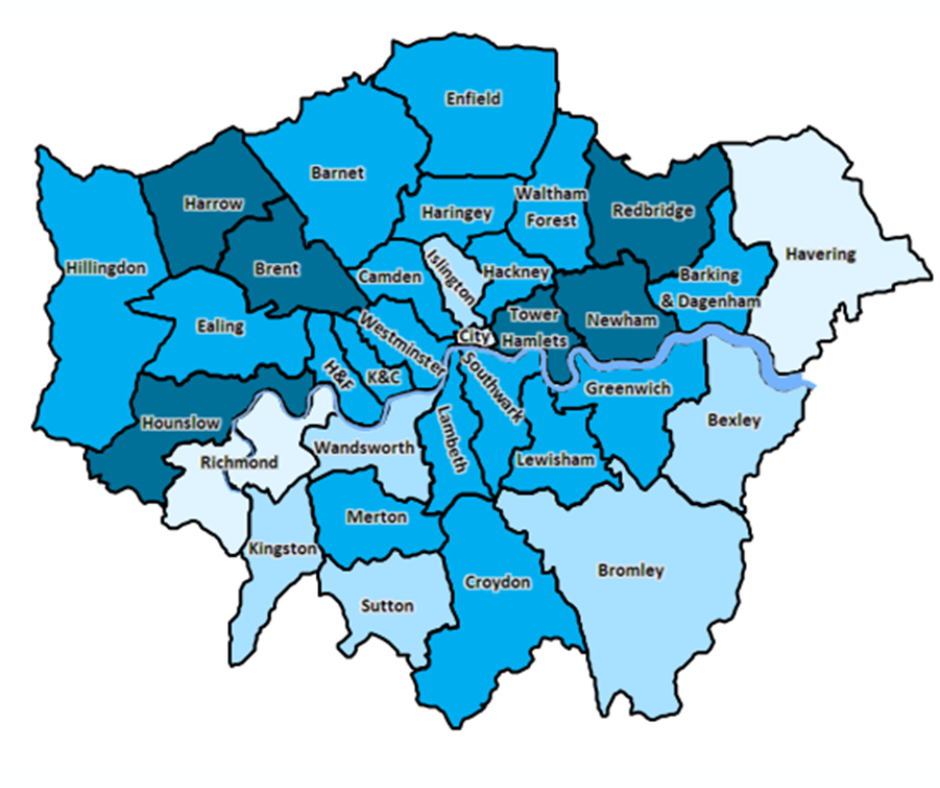
Six Integrated Care Systems
- North-East London Health and Care Partnership
- North Central London Partners in Health and Care
- North-West London Health and Care Partnership
- Our Healthier South-East London
- South-West London Health and Care Partnership
- Surrey Heartlands Health and Care Partnership
Seven Renal Units
- Barts Health NHS Trust
- Imperial College Healthcare NHS Trust
- Royal Free London NHS Foundation Trust
- Epsom and St Helier University Hospitals NHS Trust
- St Georges University Hospitals NHS Foundation Trust
- Kings College Hospital NHS Foundation Trust
- Guy’s and St Thomas’ NHS Foundation Trust
Providing kidney services across 32 London Boroughs & Surrey
There are
people in London living with Chronic Kidney Disease
London has around 15k prevalent renal replacement therapy patients.
- 6.5k people are on haemodialysis
- 15.2k people have end-stage kidney failure
- 8.7k people have had a kidney transplant
Data from the UKKA Patient Reported Experience Measures (PREMs) Survey shows patient experience is poorer in London in key metrics, such as shared decision making.
London and Surrey’s
renal units provide care to
26%
of Englands
in-centre
haemodialysis
patients
The seven adult renal centres deliver dialysis in over 45 units, delivering care to around 5,800 in-centre haemodialysis patients.
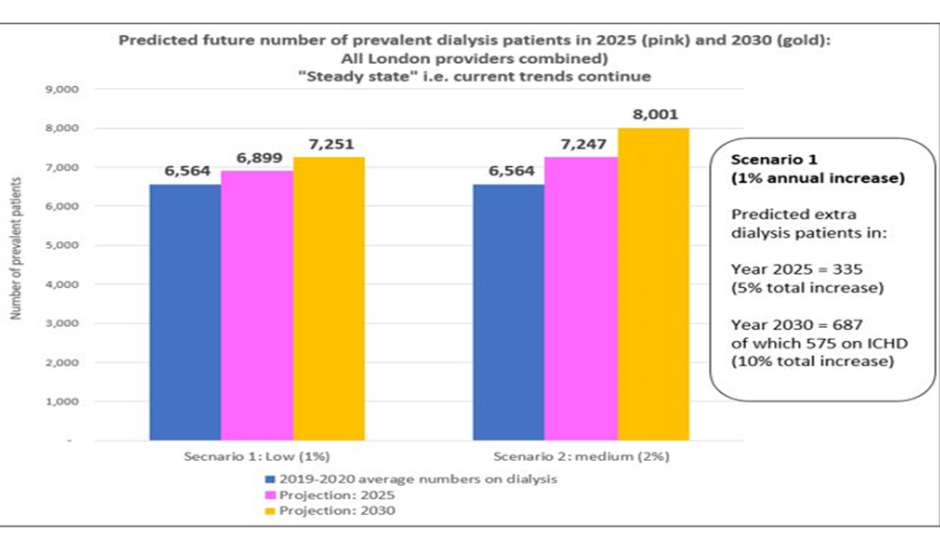
At the current rate of dialysis growth, London could have an extra 700 dialysis patients in 10 years’ time.
This would require additional capacity equivalent to Kings to accommodate.
Links to data page
and links to individual workstream pages and expert groups.
London Kidney Network equity audit: key findings
Equity of access, quality and outcomes – baseline assessment (pre-COVID, adults)
Download our full LKN Health Equity Audit findings.
Age
Inequities found:
Older people and Peritoneal Dialysis / transplant
Younger people and outpatient attendance / late presentation
Sex
Inequities found:
Women and CKD diagnosis / RRT
Young men and outpatient attendance / late presentation
Socio-economic status
Inequities found:
Patients from more deprived areas and:
- Late presentation
- Outpatient attendance
- Transplant
- Peritoneal Dialysis
Ethnicity
Inequities found:
Ethnic groups other than white and outpatient attendance / transplant
Geography
On all equity metrics there was wide variation between renal centres or Integrated Care Board areas.
Age:
The risk of developing kidney disease and also requiring Renal Replacement Therapy (RRT) increases with age, with a peak in the 75-84 year age band with a median age of 64 years. (1,2)
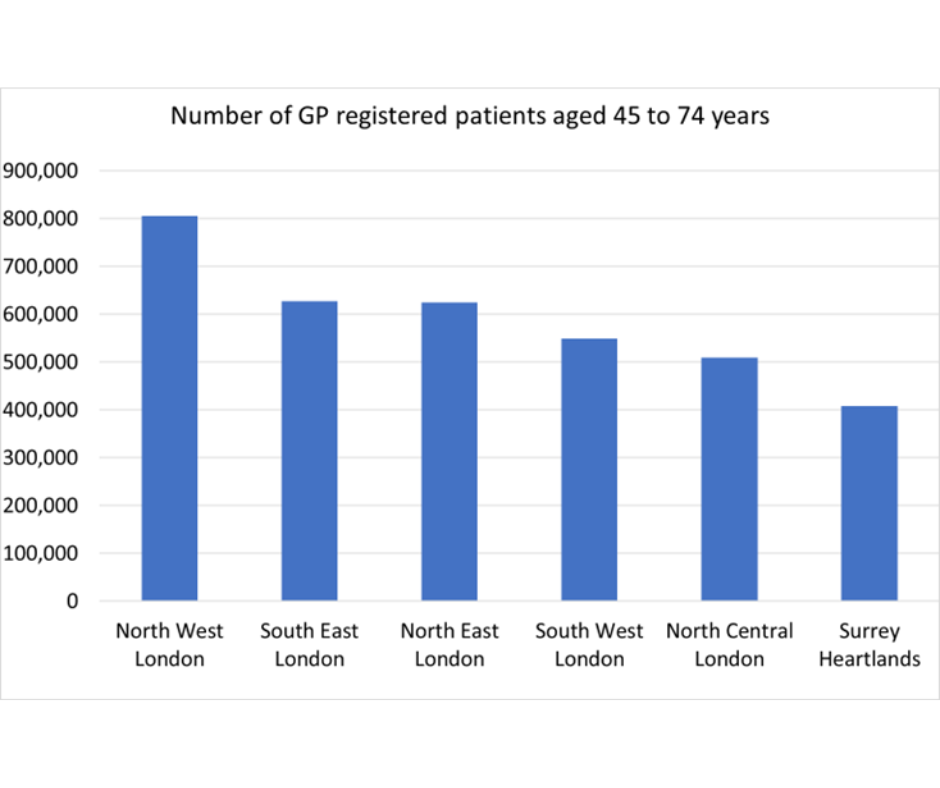
The burden of RRT service provision (in terms of numbers) falls mostly within the 45-74 year age band. The median age for the prevalent RRT population is 60 years (2)
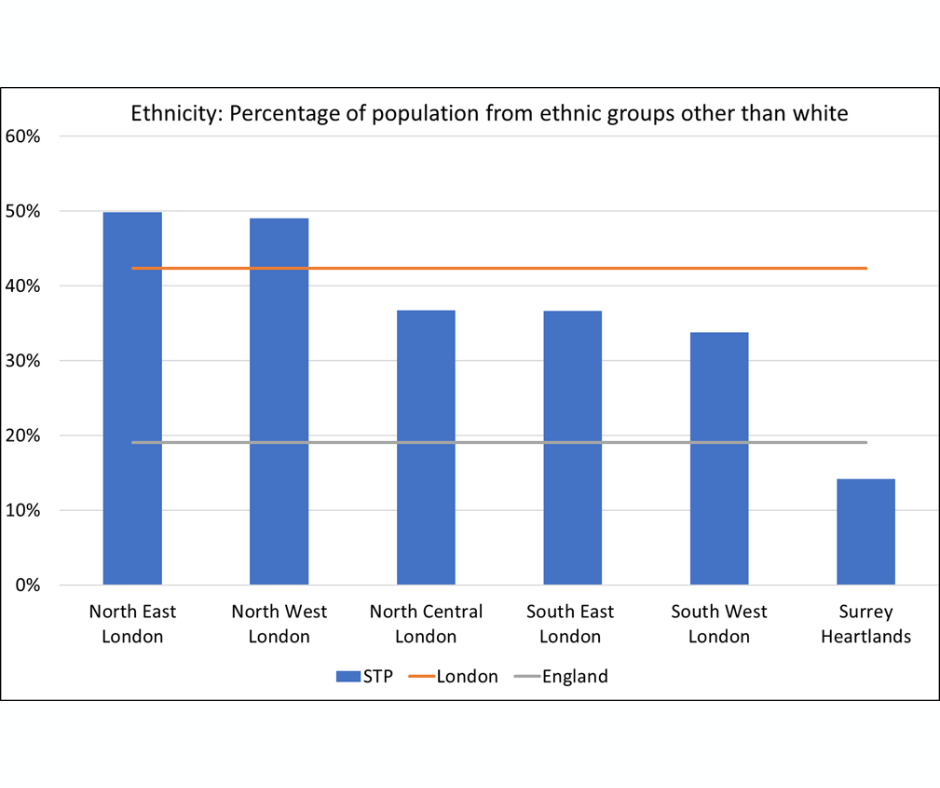
Ethnicity:
Crude incidence rates for RRT are higher amongst Black and Asian ethnic groups (2). Evidence for ethnic differences in CKD progression and outcomes is mixed (3). Evidence for poorer access to healthcare services in general for BME groups is reported (4).
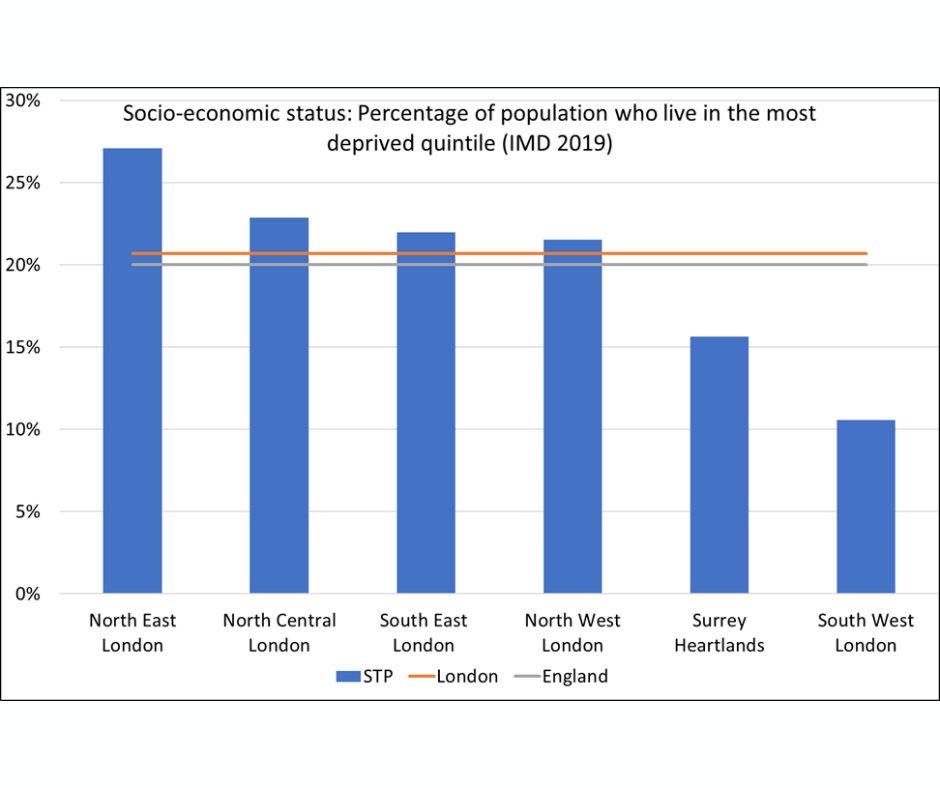
Socio-economic status:
Crude incidence rates for RRT are higher amongst patients who live in areas categorised as more deprived (2). Evidence from research demonstrates that those who are social deprived are more likely to develop CKD than their less disadvantaged counterparts (5)
Clinical risk factors:
High blood pressure is both a leading cause of and complication of CKD. It increases the chance that kidney disease will get worse (6).
Diabetes is the leading cause of kidney failure, An estimated 40 per cent of people with both type 1 and type 2 diabetes will develop CKD during their lifetime (7)
Early stage CKD is clearly a risk for developing more advanced disease as well as being a risk factor for AKI. Albuminuria is a risk factor for faster progression of CKD as well as renal failure and CVD (8)
Frailty is prevalent in patients with CKD and it is associated with an increased risk of adverse health outcomes (9)
Mental health disorders or more common among people living with kidney disease which has consequences for their ability to adhere to treatment plans (10)
Heart failure is a significant risk factor for kidney disease (11)
Population Risk Factors
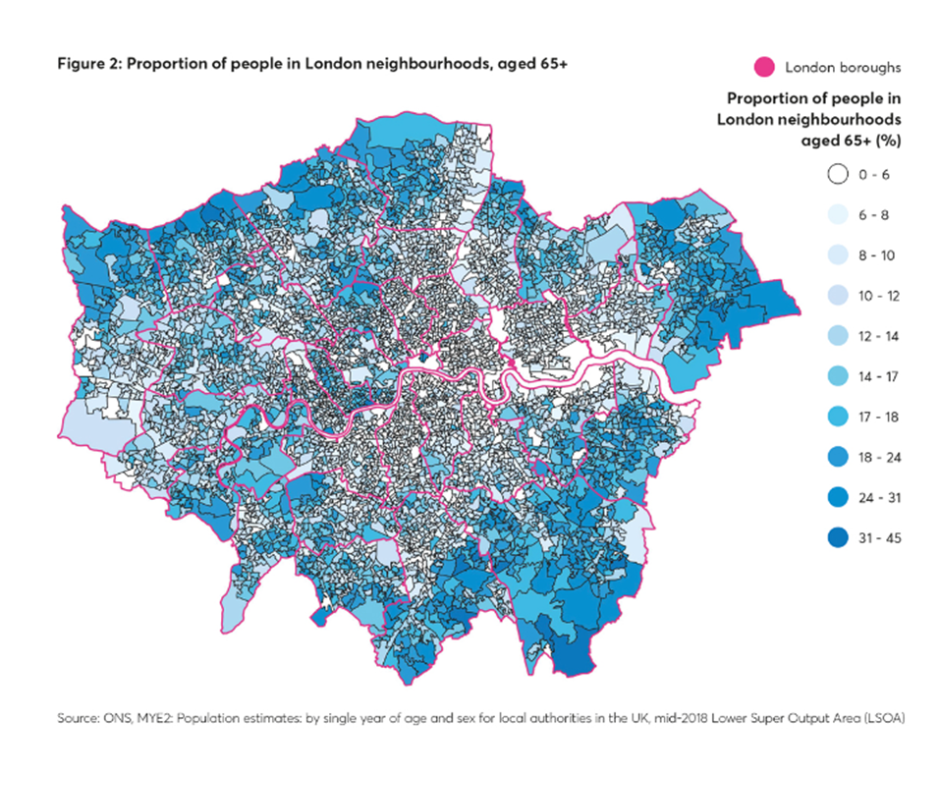
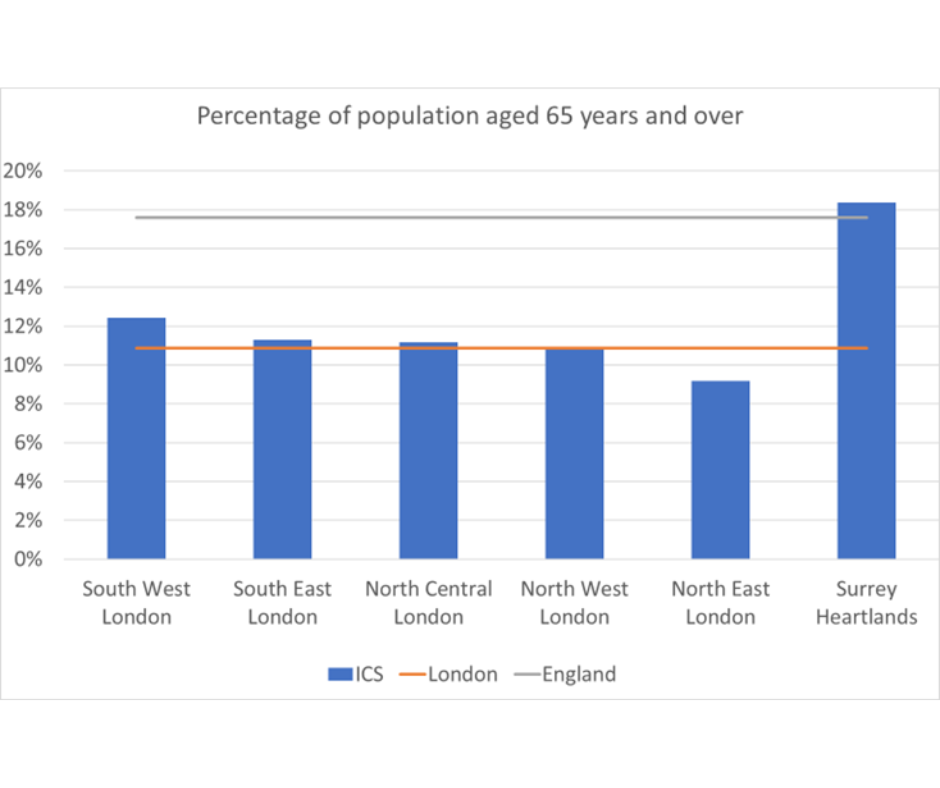
Population age-structure of London
The map below, demonstrates how the population of London varies in terms of the proportion of people aged over 65, with some areas having in excess of 30% of the population within this older age group. The two charts demonstrate age-related risk is a factor for Surrey Heartlands whereas North West London has the biggest potential for kidney disease burden in terms of absolute numbers.
Population from an ethnic group other than white
The map below demonstrates the distribution of people of different ethnicity across London (the darker colours indicate a higher % from ethnic groups other than white).
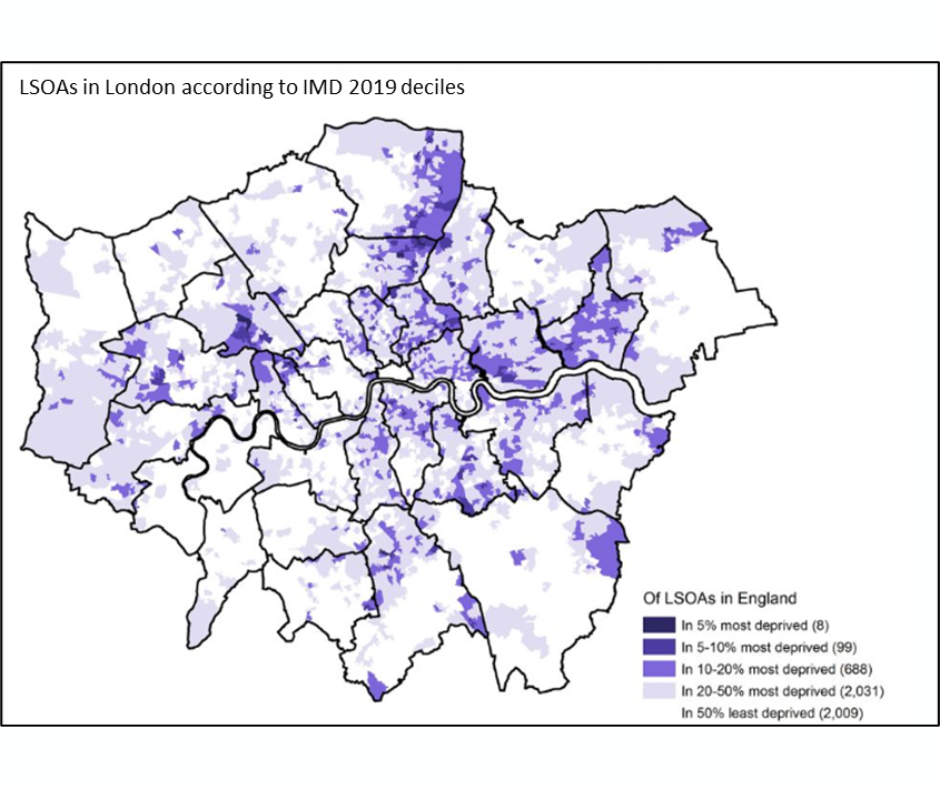
Socio-economic status (deprivation: based on the Index of Multiple Deprivation)
Overall, London has a similar level of deprivation to that of England as a whole. The number of neighbourhoods (LSOAs) in London among the most deprived 5% in England is eight out of a total of 4,835 LSOAs in London, or 0.2 per cent of London’s LSOAs. There are a further two per cent more (99 LSOAs) in England’s most deprived 10%.
However, in terms of relative deprivation within London, East London has a higher proportion of it’s population that live in areas categories as amongst the most deprived in the country. Surrey Heartlands and South West London are comparatively less deprived than the rest of London (and England as a whole).
The University of Sheffield, in collaboration with the Ministry of Housing, Communities and Local Government have produced IMD maps by Local Authority which can be downloaded here
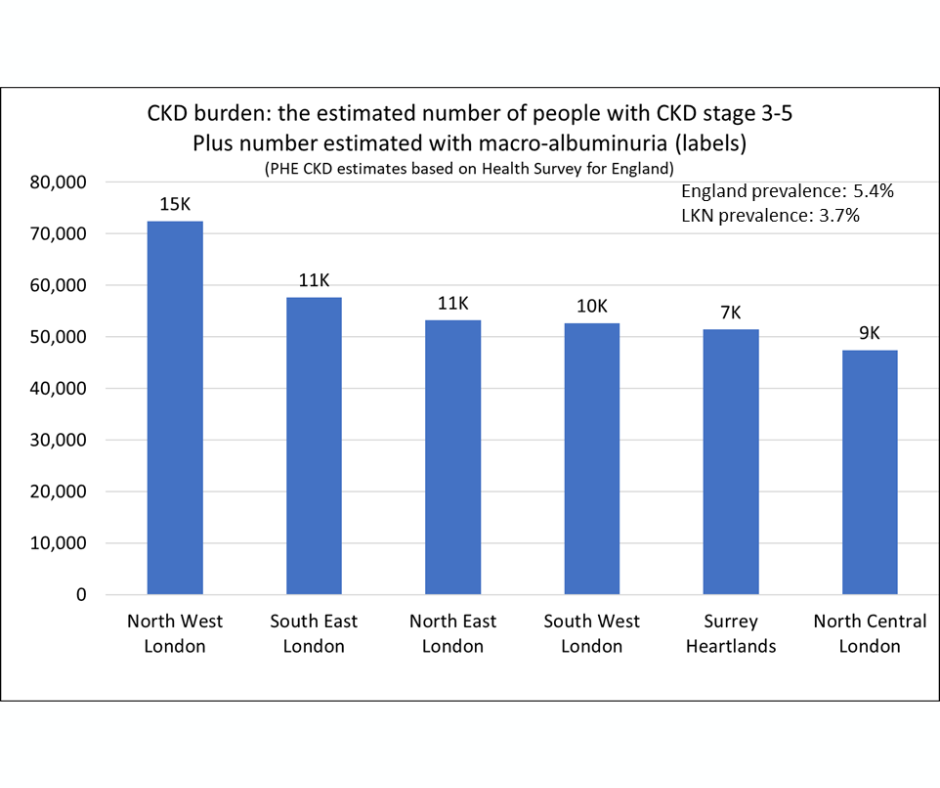
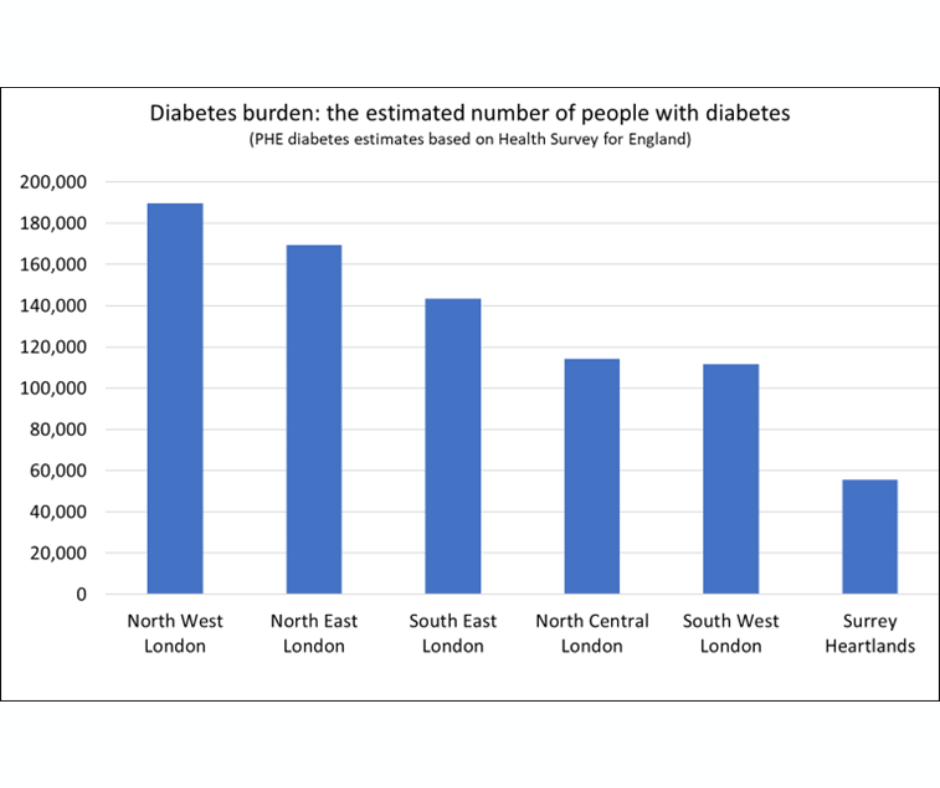
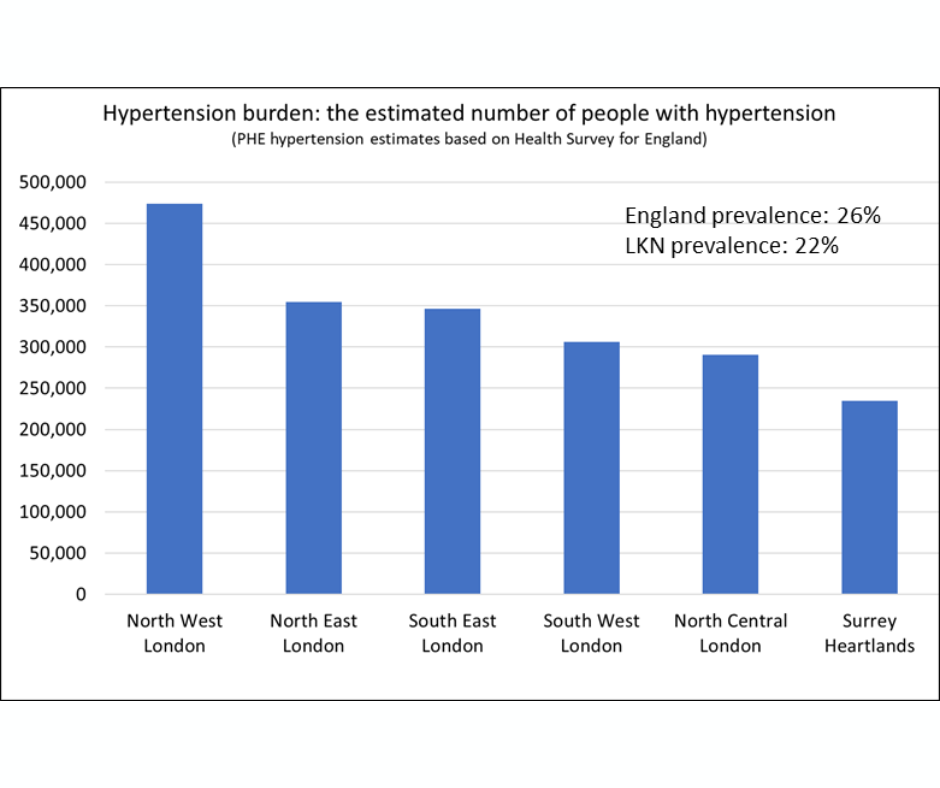
The burden of clinical risk factors
The charts show the estimated number of people to be living with CKD stage 3-5, Diabetes or Hypertension by ICS (both diagnosed and undiagnosed). These data have been estimated from national survey sources. We do not have actual data on the true prevalence of these conditions at sub-national geographies and so estimates of risk (%) cannot be shown. However, the burden (i.e. the estimated number of people) of these conditions is still of interest for service funding and planning purposes.
It can be seen that the pattern between ICSs is generally driven by a function of population size, with the more populous ICS areas having the biggest burden. The age structure of the population has been taken into account in these estimates but other factors have not, such as ethnicity and deprivation. Therefore, these estimates should be interpreted alongside the ethnicity and deprivation information on previous slides.
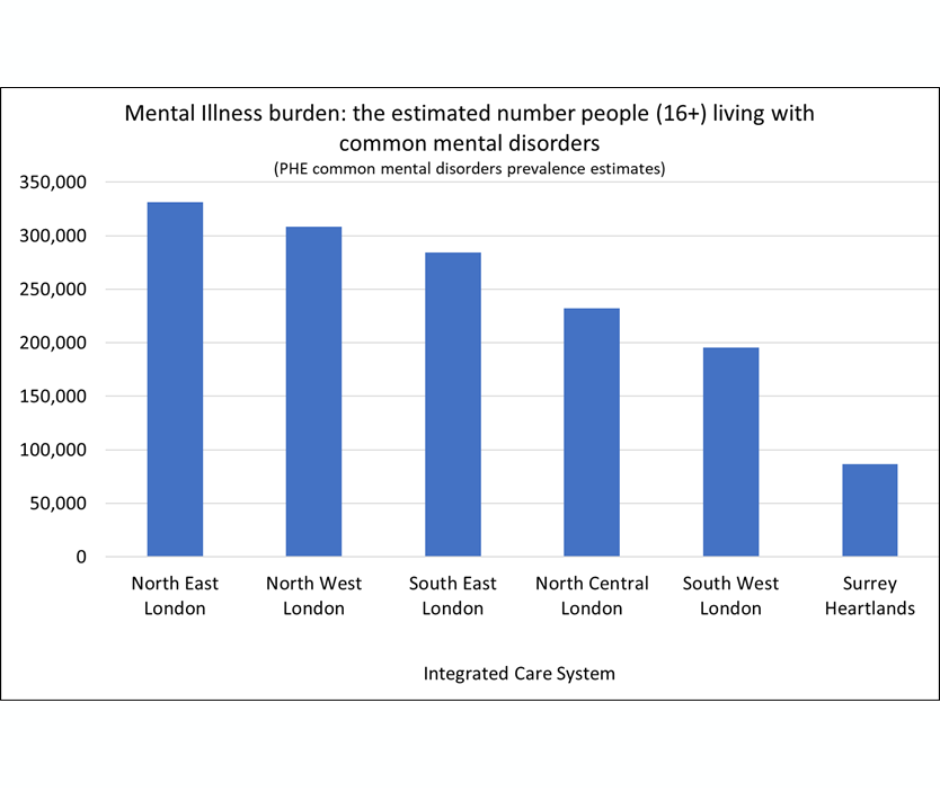
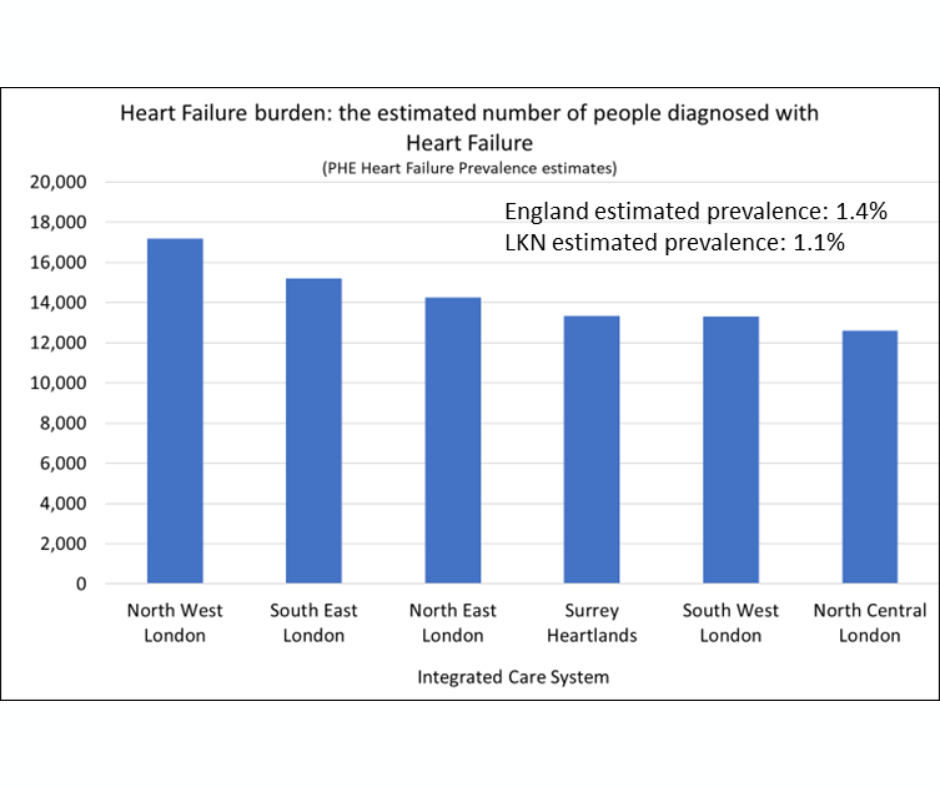
The burden of clinical risk factors (continued)
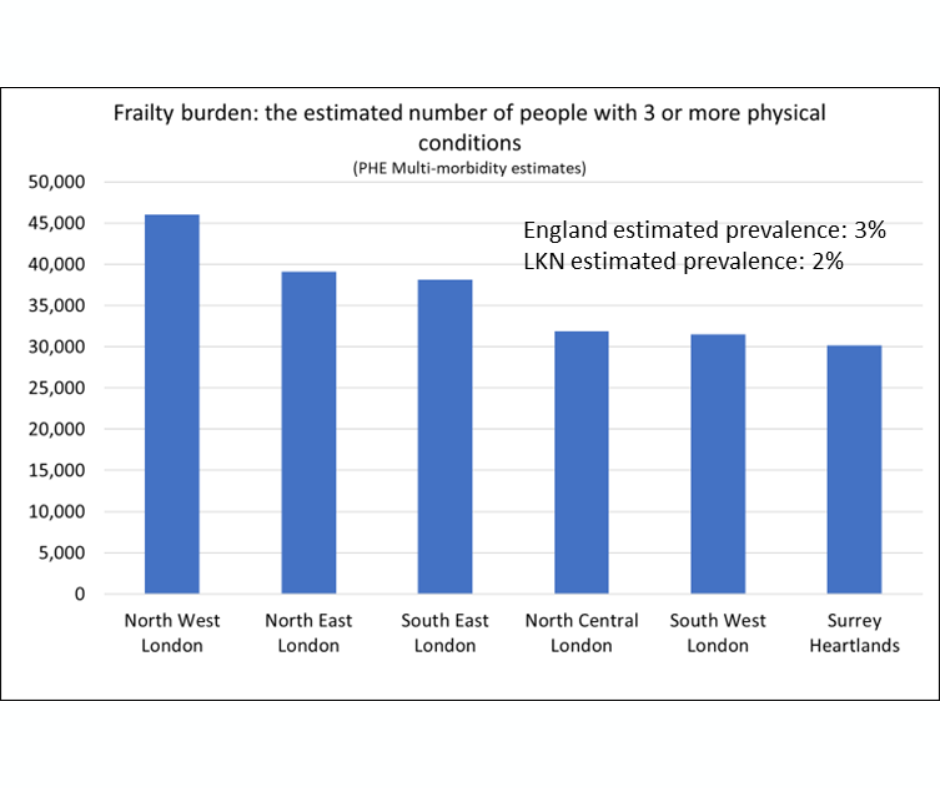
The charts show the estimated number of people to be living with frailty (multi-morbidity), Heart Failure or Mental Illness by ICS (both diagnosed and undiagnosed). These data have been estimated from national survey sources. We do not have actual data on the true prevalence of these conditions at sub-national geographies and so estimates of risk (%) cannot be shown. However, the burden (i.e. the estimated number of people) of these conditions is still of interest for service funding and planning purposes. The age structure of the population has been taken into account in these estimates but other factors have not, such as ethnicity and deprivation. Therefore, these estimates should be interpreted alongside the ethnicity and deprivation information on previous slides.
It can be seen that the pattern is generally driven by a function of population size, with the more populous ICS areas having the biggest burden. Although this is not always the case, for example, North East London is estimated to have a high burden of mental illness relative to population size.
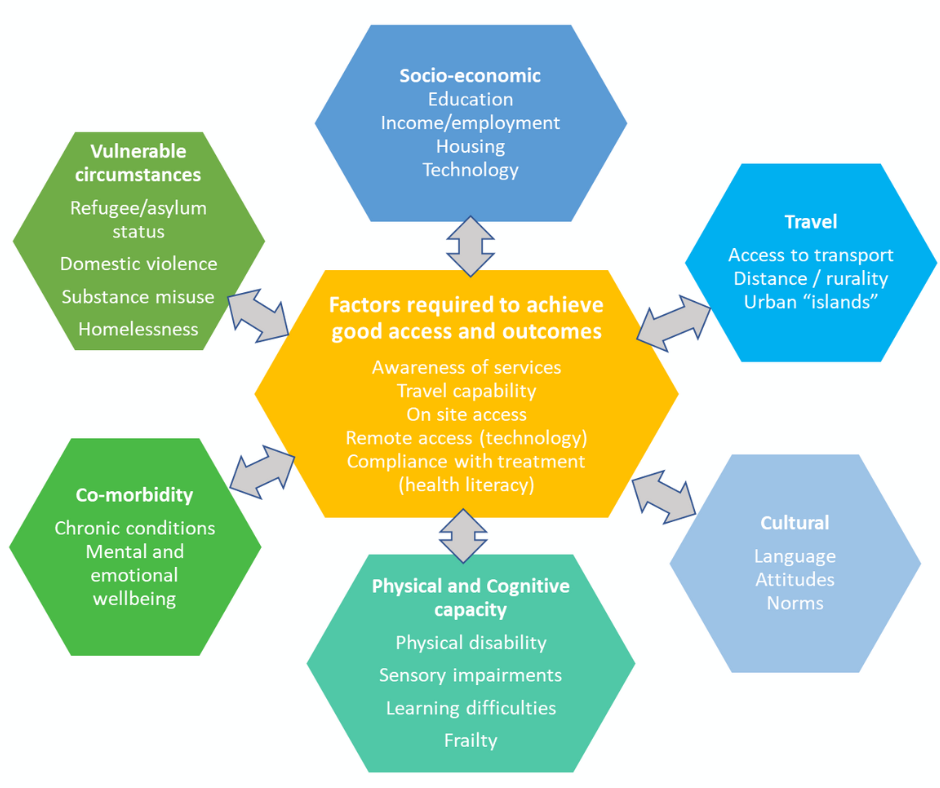
Potential barriers to access and good outcomes
This illustration represents some of the factors that may create barriers to being able to access services and/or achieve good health outcomes for some population groups.
Local systems may wish to explore the distribution of these factors within their populations in relation to those at risk of/requiring use of renal services. Links to the Joint Strategic Needs Assessment for each Borough have been provided in the final slide.
On the following slides, Borough level data for a selection of these factors are shown for London only.
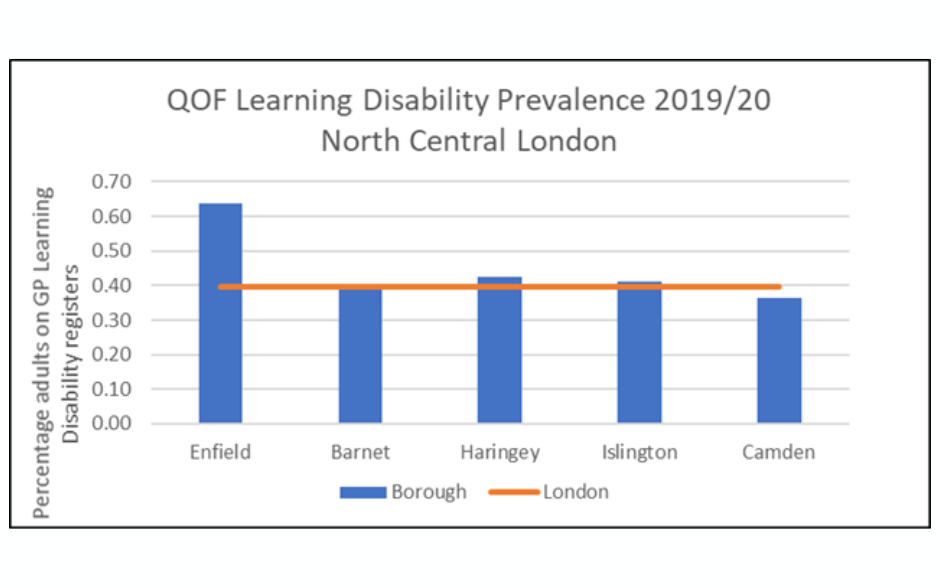
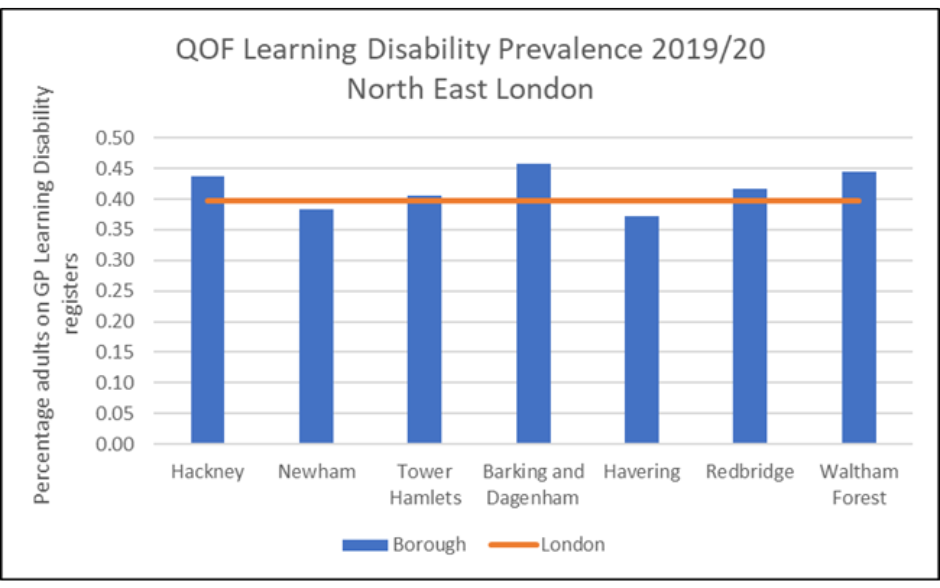
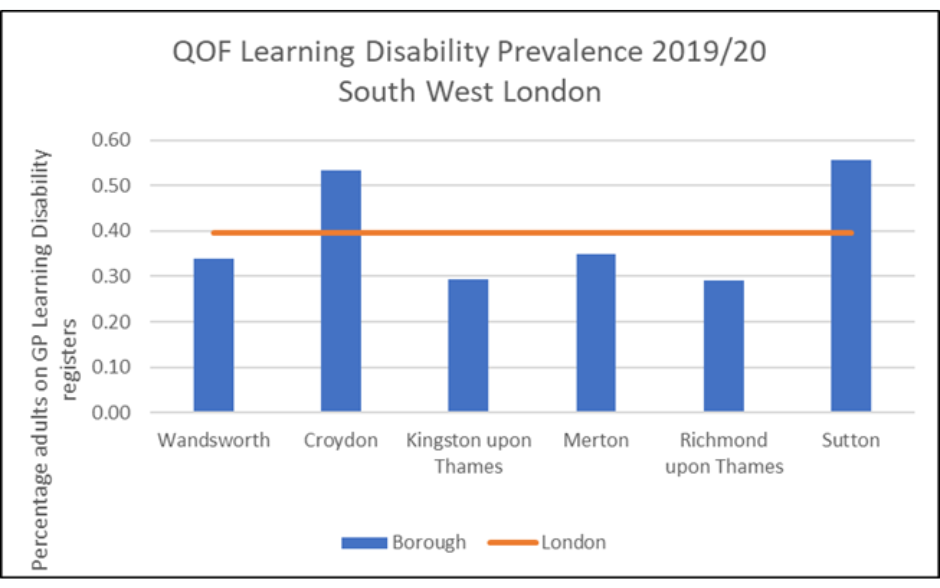
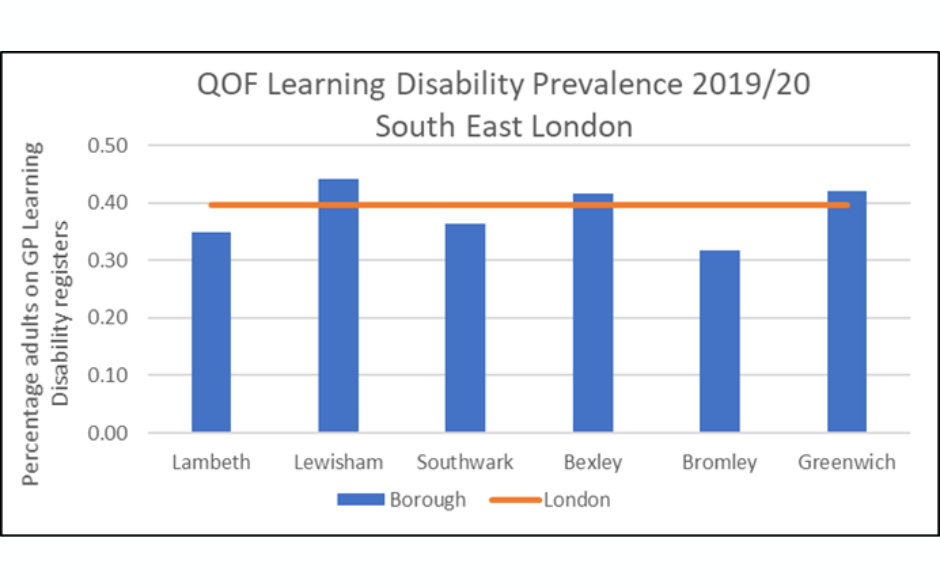
Learning Disability Primary Care Registers


Data in the LKN
At the heart of decision-making and improvement planning
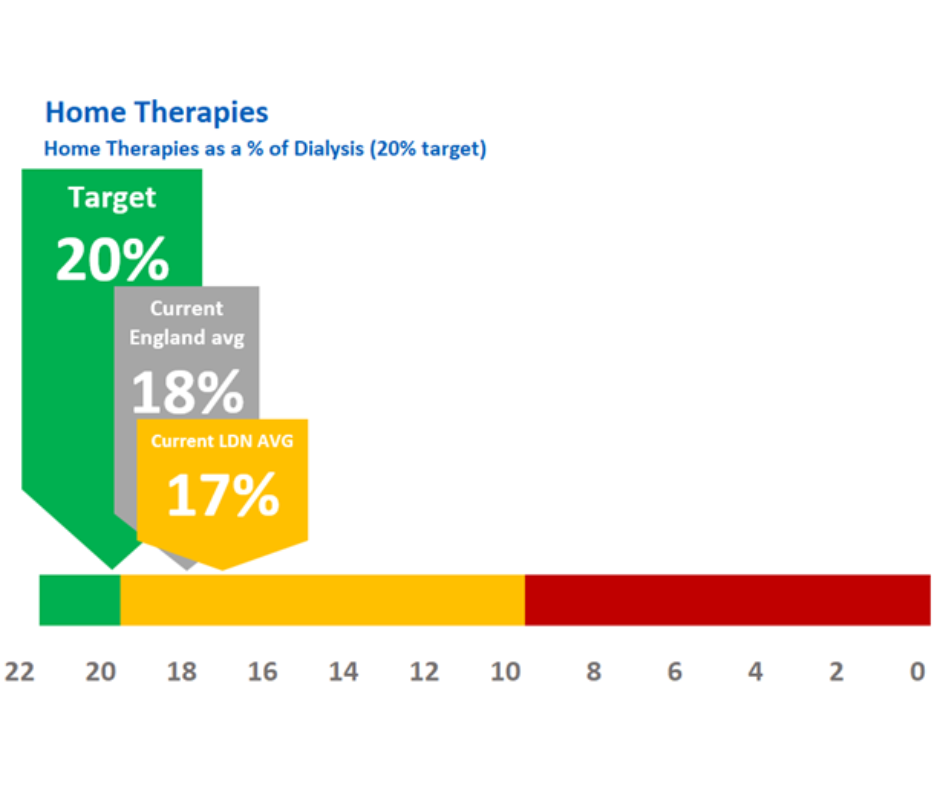
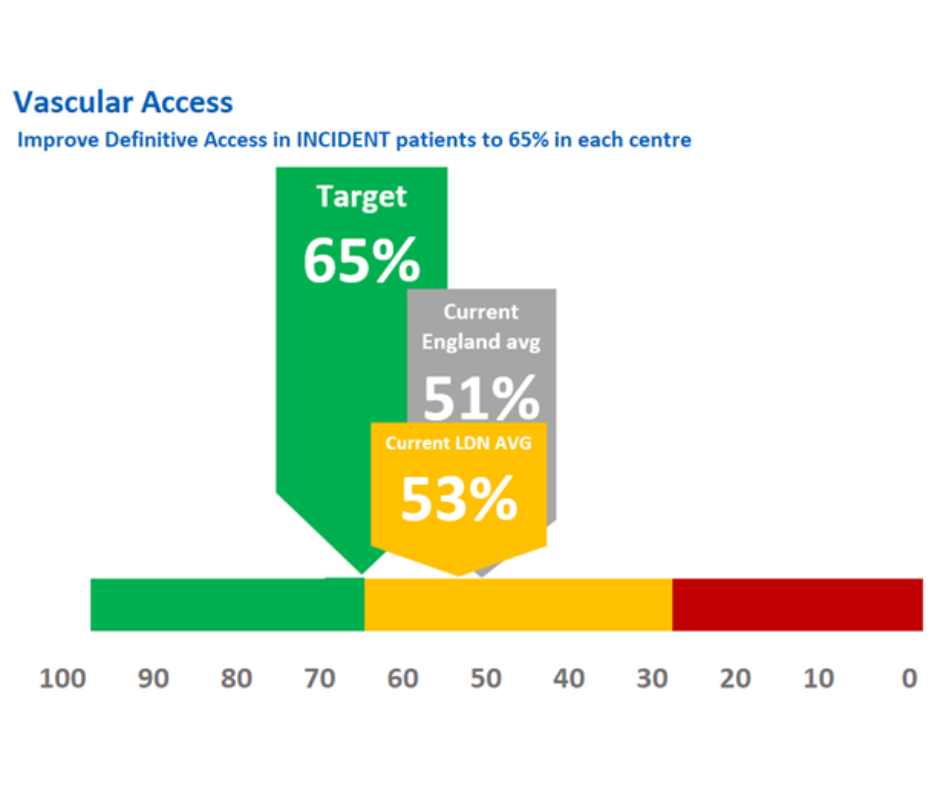
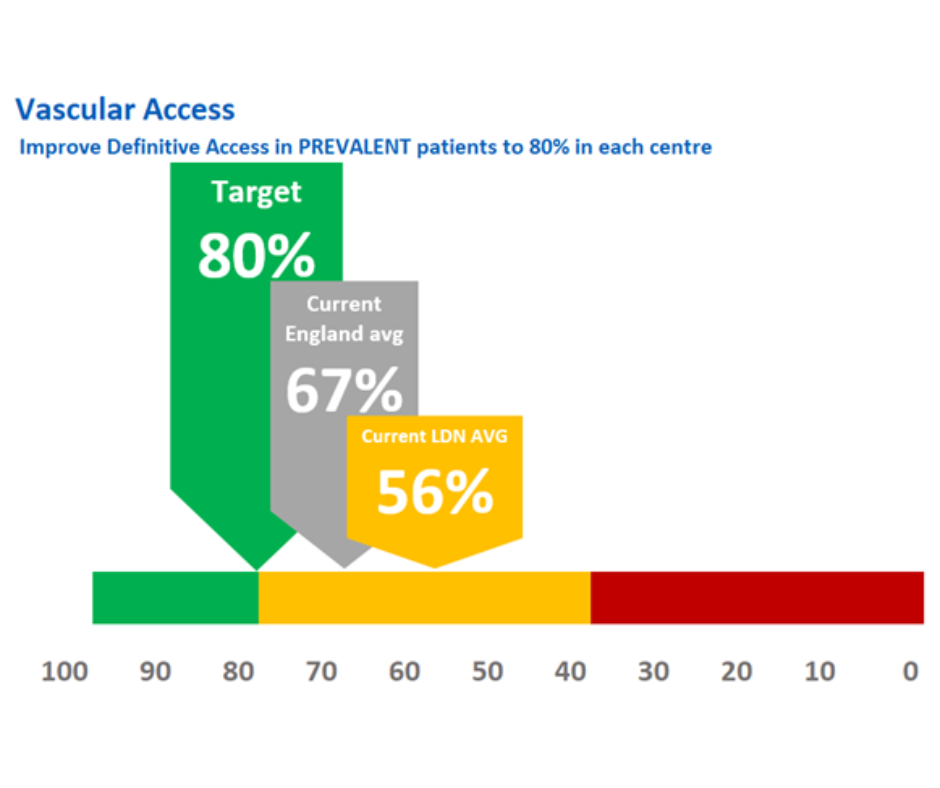
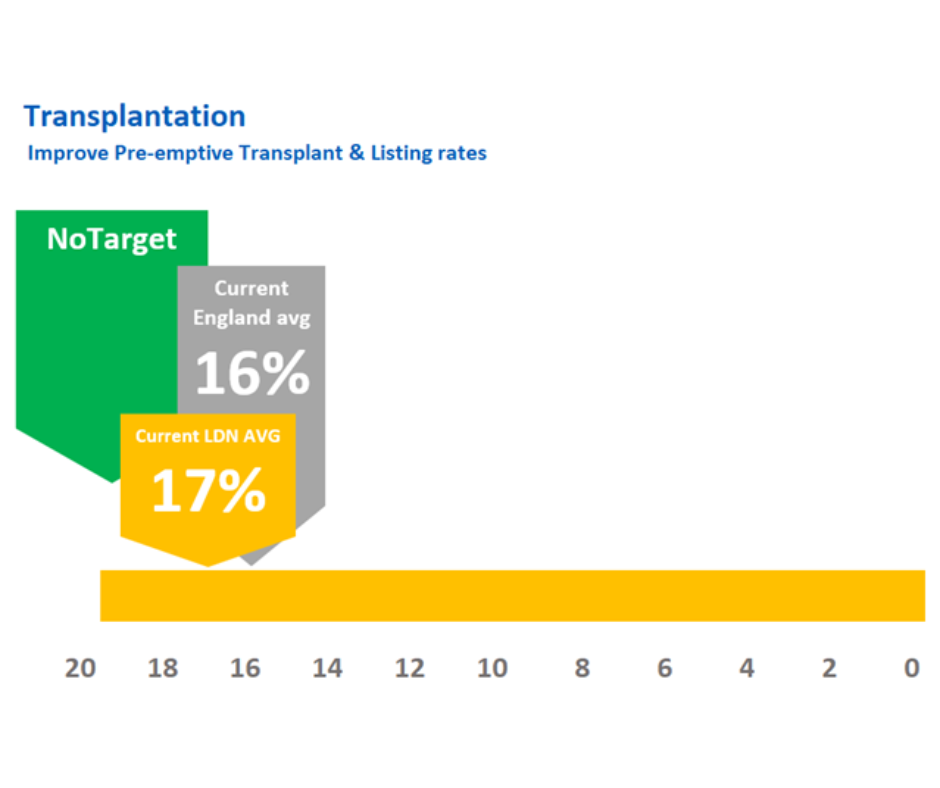
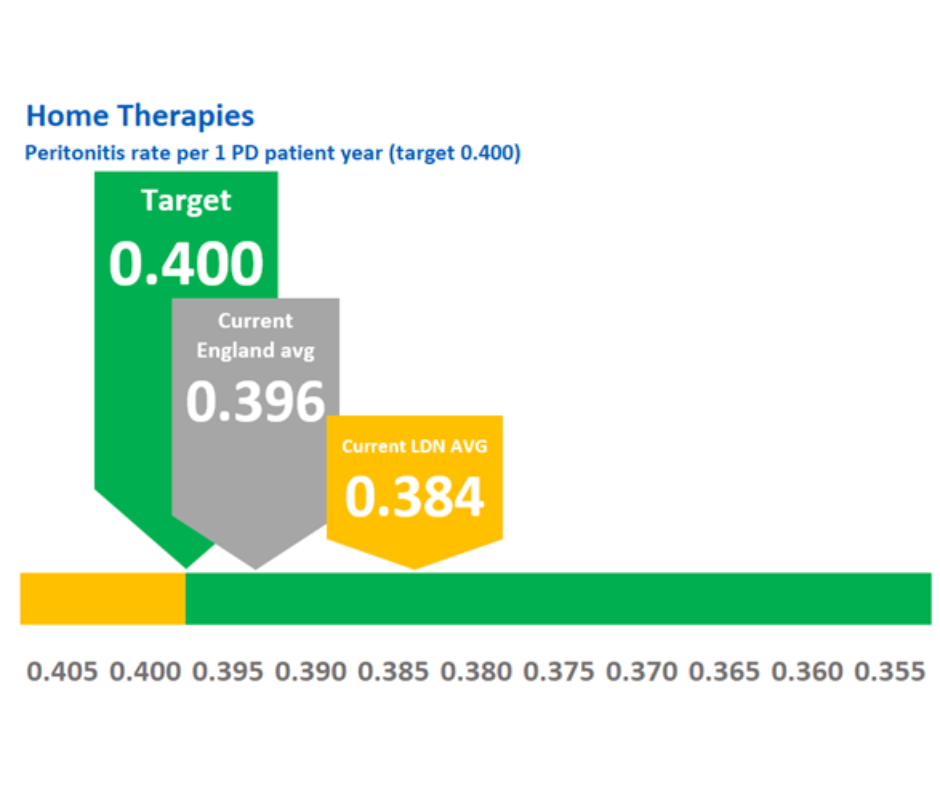
How does London compare to agreed targets and to national average in key metrics?
Our workstreams’ aims, objectives and workplans have been developed to support our renal centres to
- Reach targets set by RSTP and GIRFT, and
- Deliver measurable quality improvement across London
Here, we show our combined renal unit position as compared with national position and target position for Transplantation, Home Therapies and Vascular Access.
We are developing our approach to focus on improving the use of data to inform decisions and ensure that we directly target health inequalities in the kidney pathways of care.
Creating an LKN Dashboard
Sharing robust data is key to showing difference and hence identifying good practice and areas of unwarranted variation.
- We developed a comprehensive data dashboard which was first published in December 2021 using agreed metrics, by workstream, at Trust level. It currently pulls data from existent sources into one place.
- This will be further developed early in 2022/23 to show ICS level data.
- The LKN Clinical Information Group (CIG) will develop this yet further to include additional workstream metrics
GIRFT/RSPT Mapping Report
We mapped the LKN workplans against Renal Service GIRFT Report and the RSTP to ensure we:
- addressed all priority actions for networks in year and into 2022/23
- work collaboratively with and responsively to national data workstreams e.g. RSTP
- address unit level responsibilities though our workstreams and so:
- minimiserepetition
- share learning, and provide a pan-London solution to issues
RRT Demand capacity
Demand for renal replacement therapy has increased steadily over the last five years. In 2021/22 we showed that likely demand in 5- and 10-years times will outstrip capacity by around 700 patients, equivalent to a unit the size of King’s College Hospital.
We will work with units and ICSs in 2022/23 to seek solutions, including through improvements in transplantation pathways and CKD early detection and management.
Primary Care Network level data for pilots
As part of the CKD pilot development, we needed to show at PCN level where there was greatest variation in actual against expected CKD prevalence and medical management against guideline standards.
Working collaboratively with our partners in NHSE/I data presented in a RAG format, provided a clear basis for inclusion with the in the planned pilot project. We identifed PCNs with most potential to: improve CKD outcomes for patients; reduce variation; and slow growth in demand for RRT.
